Verified, Real-Time Data Solutions
Powered by Verisys
Verisys empowers healthcare organizations with real-time, verified data solutions for compliance, credentialing, and risk mitigation. Our advanced tools ensure patient safety, streamline hiring, manage payment integrity, and enhance clinical compliance.
Healthcare Provider Compliance Data Solutions
Transforming healthcare compliance programs with better data delivered where and when you need it.
The Industry Leader in Healthcare Compliance Data
Better Data. Better Decisions. Better Outcomes.
Real-Time, Verified Data
Drive your compliance program with the power of real-time, pristine data.We deliver verified provider data with over 99.95% accuracy, significantly outperforming competitors in both speed and reliability by 30+%.
Scalable Data Solutions
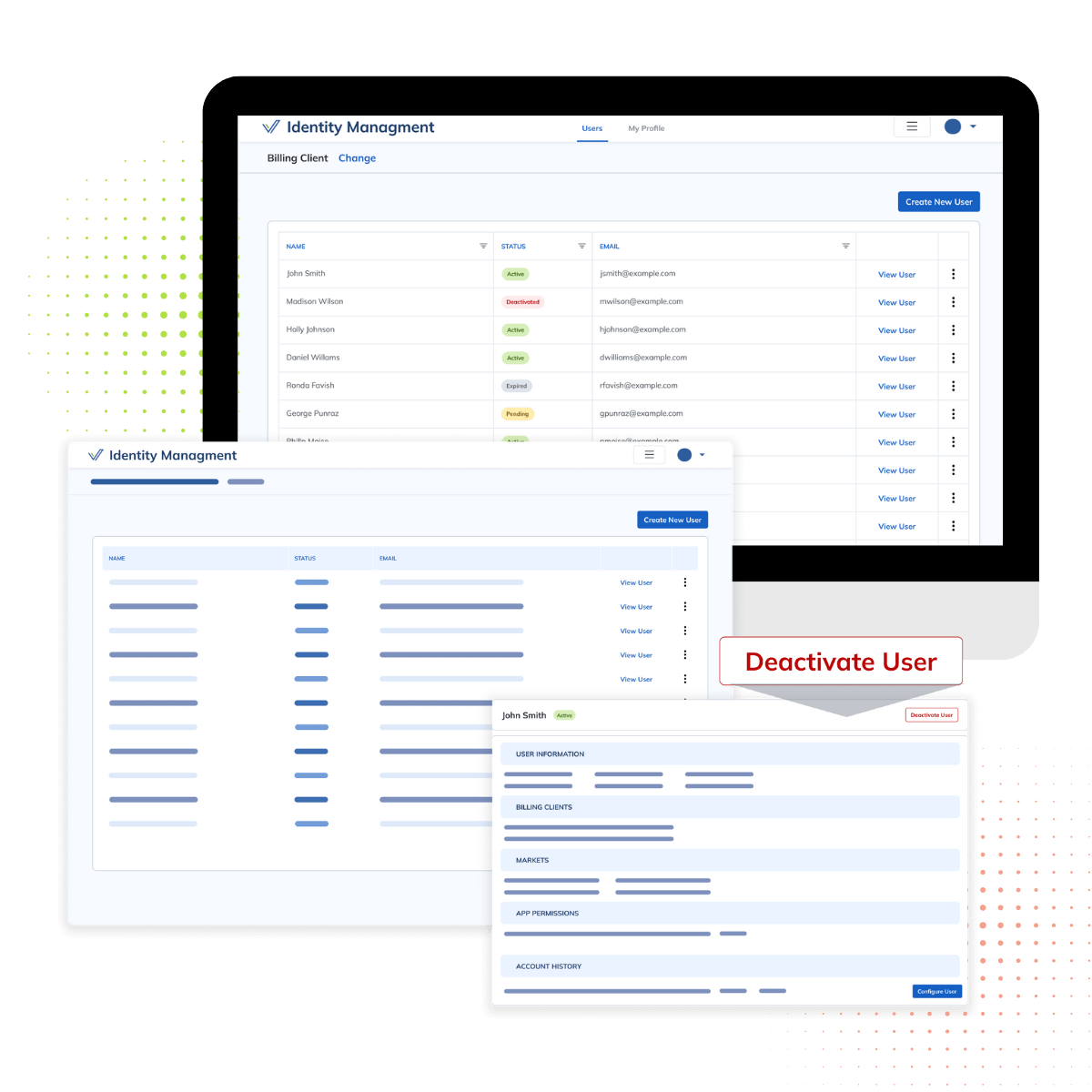
The most comprehensive data coverage across ALL provider types.Our credentialing and compliance management system offers comprehensive data coverage across all provider types. Verisys' solutions are designed to scale seamlessly, supporting healthcare organizations in meeting credentialing requirements and managing provider documents effectively. Automated data updates ensure continued compliance and prevention of credentialing lapses.
Optimized Outcomes
Seamless integration into preferred workflows enhancing operational efficiency and maintains compliance with medical regulations.Verisys provides healthcare compliance solutions that consolidate data across systems, allowing healthcare organizations to replace point solutions with a unified, comprehensive compliance management platform. This reduces operating costs, ensures trust, and supports quality patient care.
What Our Clients Are Saying

Brenda J. W.

Dave H.

Jimmy W.
There are a lot of positive attributes. I used Verisys for licensure monitoring for my practice and used it to access healthcare practitioner data profiles for my practice needs. I like the customer service, and they go above and beyond in providing personalized service for my practice needs.

Anish D.


Optimized Compliance Powered By Verisys
The Process:
Data Curation
We collect and curate pristine datasets, powering healthcare compliance solutions. Verisys data management mitigates risks and ensures comprehensive healthcare compliance solutions.
Proprietary Matching & Verification
Verisys' credentialing experts match provider data to curated profiles, ensuring compliance with healthcare industry standards. Through our proprietary data verification process, we achieve a 99.95% accuracy rate, helping healthcare organizations implement advanced compliance programs.
Real-Time Monitoring
Continuous monitoring powered by Verisys ensures compliance in real-time. Our automated compliance solutions mitigate credentialing issues, preventing risks and safeguarding healthcare organizations.
Compliance Optimization
Verisys helps healthcare organizations implement and manage comprehensive healthcare compliance solutions, ensuring effective reporting and clinical compliance.
Our healthcare compliance solutions are designed to provide effective insights, ensuring safe, high-quality patient care.
Operational Excellence in Healthcare Powered by Verisys
Comprehensive, real-time data products to help streamline credentialing processes, enhance payment integrity verification, and ongoing monitoring, making compliance processes more efficient and accurate.

(Sanctions, Exclusions, Debarments, License Disciplinary Actions)
Maintain screening and monitoring compliance.Maintain healthcare compliance and prevention of sanctions with Verisys FACIS. Our advanced compliance solutions screen and monitor employees, physicians, staff, vendors, and providers for exclusions, debarments, and disciplinary actions across all jurisdictions.
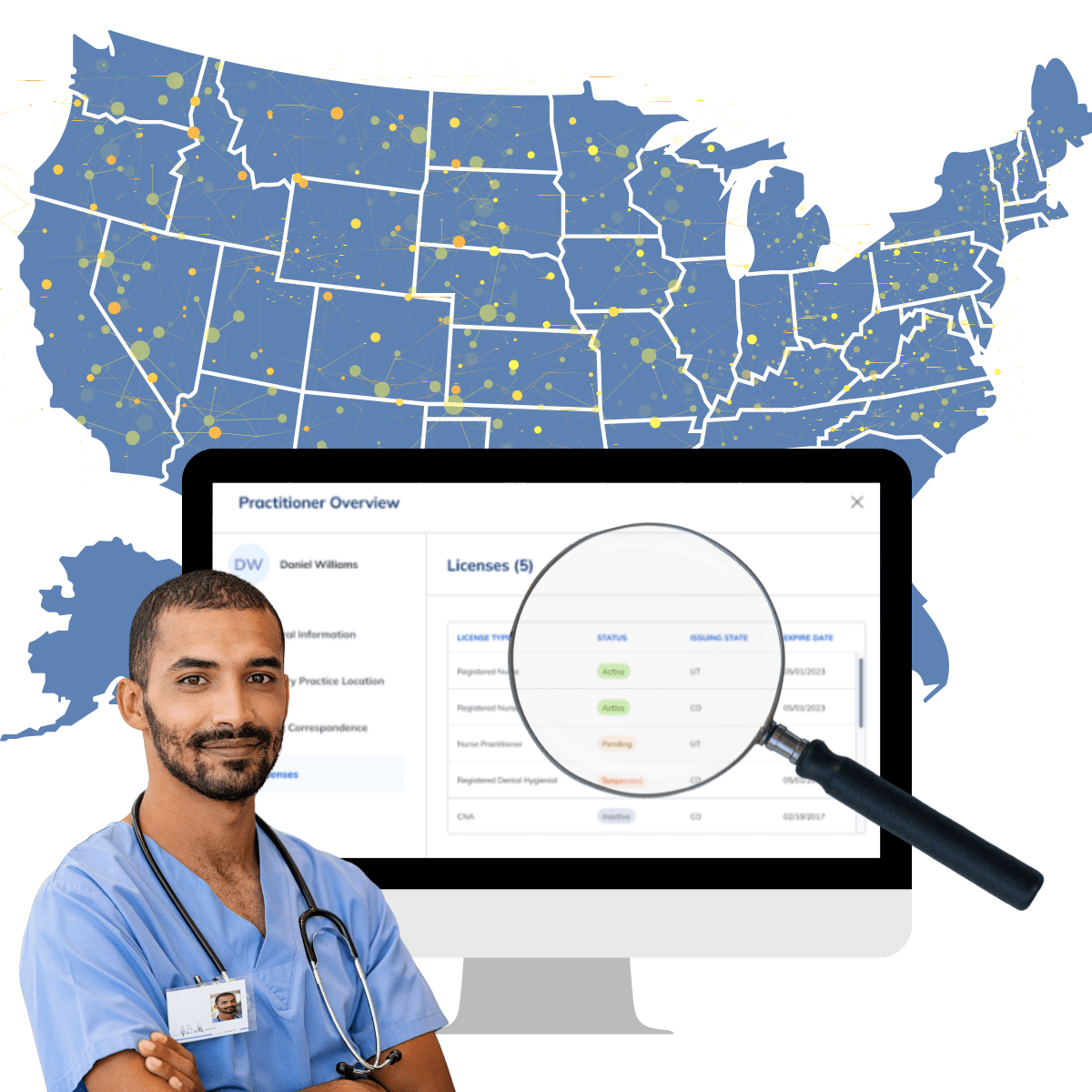
Licensure
Screen and monitor licensure for all provider and allied professional license types in all U.S. states and jurisdictions.
Verisys provides a complete licensure solution, including the ability to identify and report against all licenses held by a provider (current and historical), as well as verifying and monitoring each license for status, expiration, renewal, scope expansion and license disciplinary actions in every U.S. state and jurisdiction. Our LicenseCheck data is 30% more actionable than other market solutions and delivered with >99.95% accuracy.
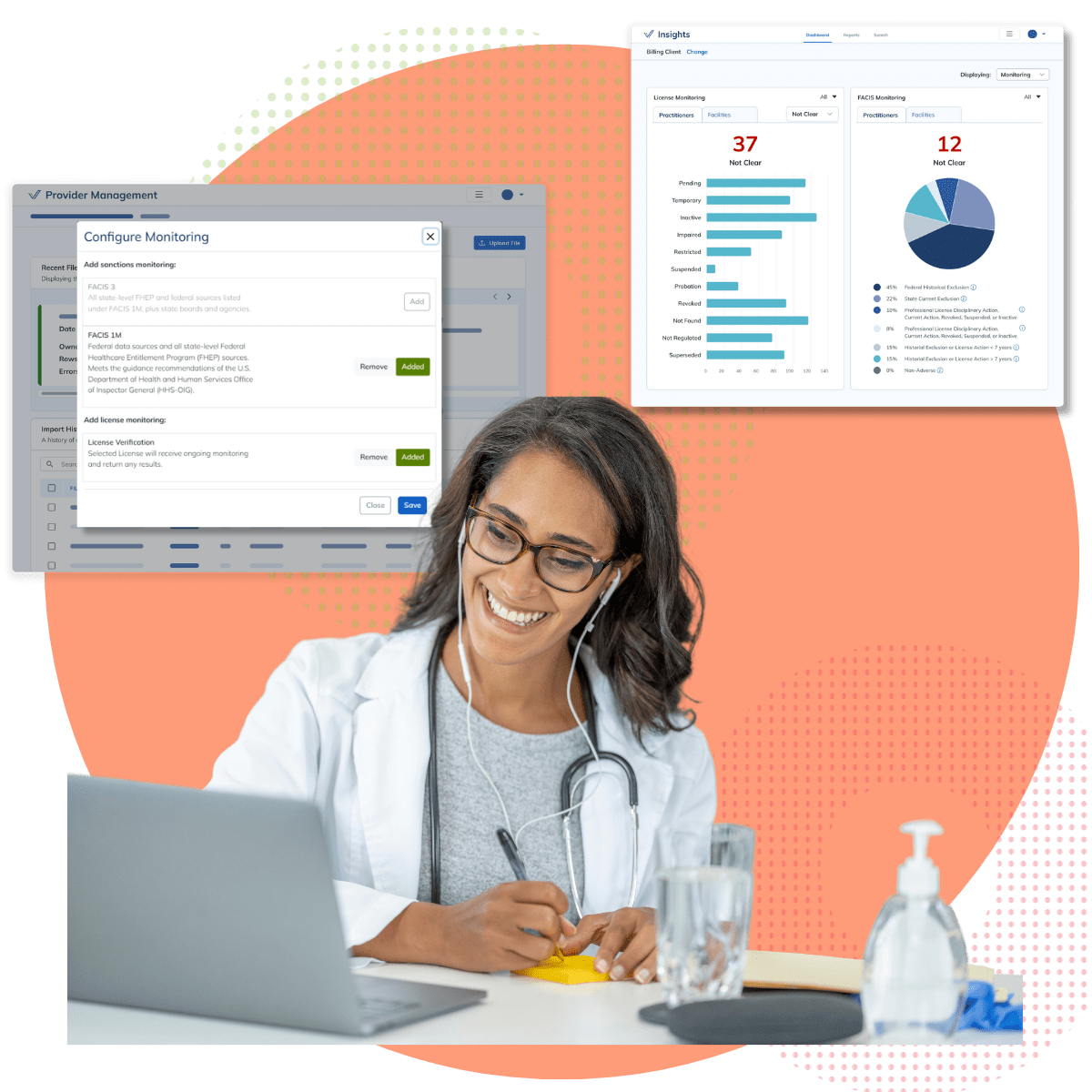
True Monitoring
Monitor sanctions, exclusions, debarments, and credentials for expiration, renewal, scope expansion and status change. Our comprehensive solutions improve data accuracy and security.VerisysWatch ensures continuous monitoring of provider credentials, sanctions, and licensure updates. Our healthcare compliance solutions deliver alerts on adverse actions, ensuring healthcare organizations remain compliant with evolving standards and regulatory changes.
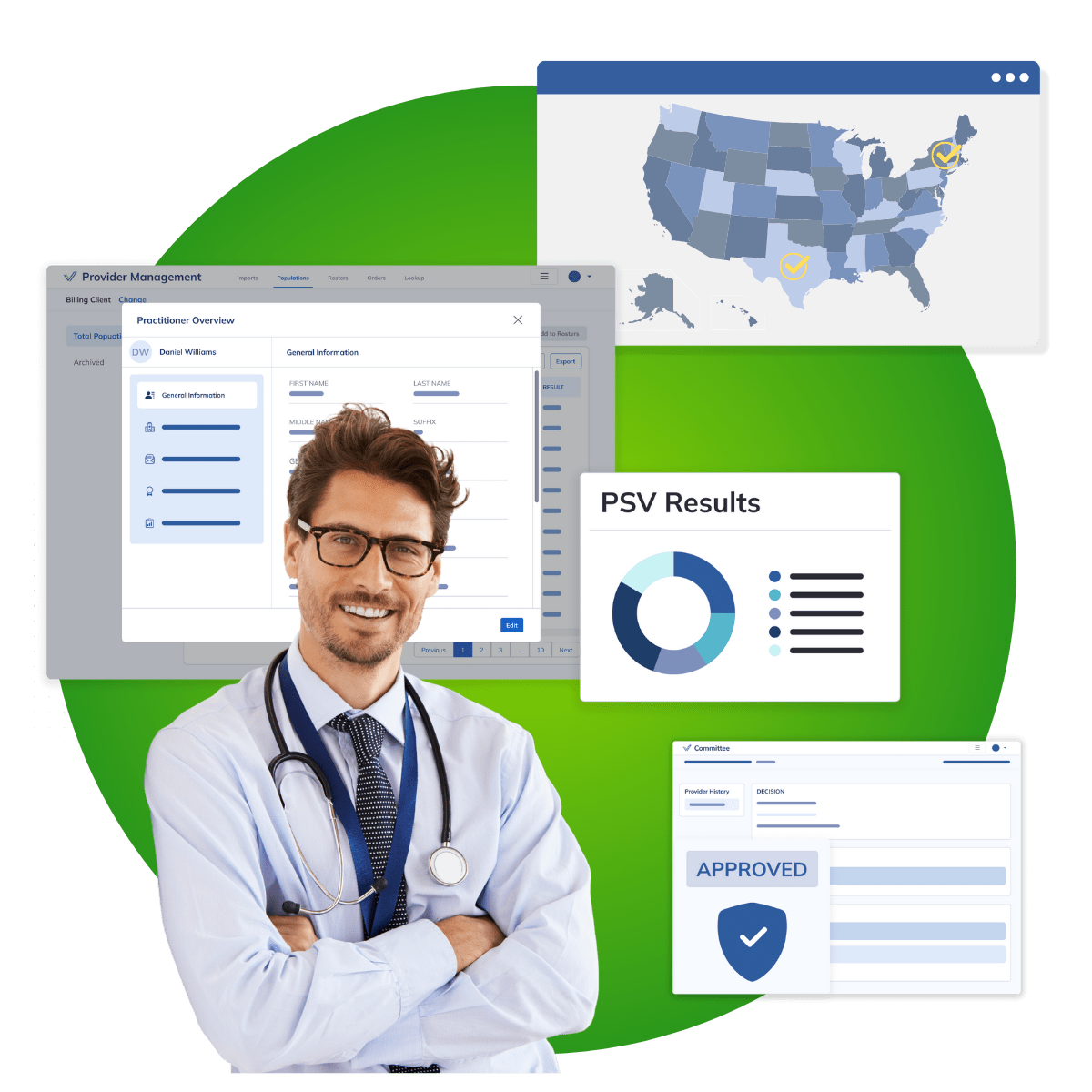
Credentialing
Verisys supports healthcare organizations with comprehensive, automated credentialing solutions that ensure providers meet regulatory standards. Our solutions streamline compliance management, mitigate credentialing issues, and ensure safe, quality healthcare delivery.Verisys CredCheck can support ongoing, perpetual credentialing of your providers with data delivered into your in-house credentialing process, an existing credentialing tool or platform, or through a fully outsourced model. Verisys completes more than two million outsourced credentialing events annually, with millions more supported through other credentialing tools, in-house programs, and monitored credentials between credentialing events. In hospitals, health systems, health plans, pharmacies, and government spaces, we are able to support credentialing, at scale, for all enrolled and allied provider types in all U.S. states and jurisdictions.
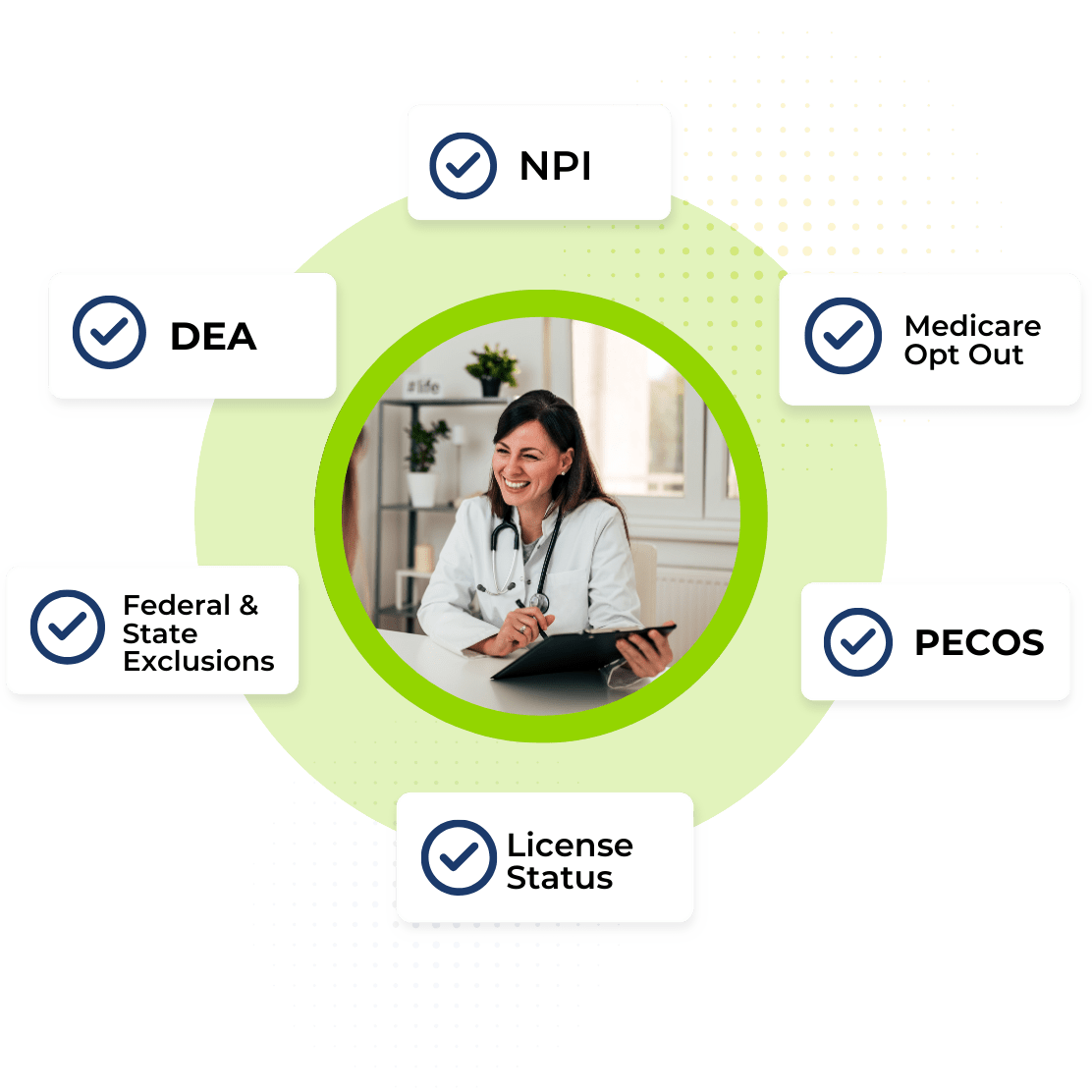
Payment Integrity & Real-time Provider Eligibility
Know in real-time if a provider is eligible to provide or schedule services, badge into your facility, receive reimbursement, submit a prescription and whether your organization should submit for reimbursement for services performed.Verisys EligibilityCheck delivers a real-time view of a provider or prescriber’s eligibility on a date of service, including Exclusion status, License Status, DEA Status, Medicare Opt-Out, and Medicare Enrollment (PECOS). This service delivers data when you need it and can be easily integrated into tools you already use today for processing claims, filling prescriptions, processing benefits, badging providers into a facility, policy underwriting, ordering and referring provider screening, and provider staffing/recruitment.
Master Provider Data Management
The Verisys data curation and management processes support data cleansing, normalization, and augmentation of high volume datasets supporting provider directories, enrollment reporting, prescriber files, ordering and referring provider files, state prescription drug monitoring program reporting, and will standardize data formatting, compare and contrast data to ensure accuracy and augment data to include critical information such as phone numbers, addresses, and license status to streamline complex data processes.
Compliance Built to Meet the Highest Standards
No matter which credentialing standards you follow, Verisys is equipped to meet them with precision. From NCQA to The Joint Commission, our expertise ensures your organization stays compliant and ahead of the curve. With Verisys’ compliance solutions, healthcare organizations can enhance their care services through improved compliance strategies.
NCQA Credentialing
NCQA credentialing standards are most common standards utilized. Verisys is an NCQA accredentied CVO. Our data helps your organization meet NCQA standards.

NCQA Credentialing & Recredentialing
As an NCQA-accredited CVO, Verisys helps you achieve and maintain NCQA credentialing standards, ensuring compliance with the strictest requirements.

The Joint Commission Credentialing
We support organizations in meeting The Joint Commission’s credentialing requirements, providing a comprehensive approach to compliance.

URAC Credentialing
Verisys delivers solutions that meet URAC standards, helping your organization maintain oversight and accountability in every credentialing step.