– The best resource for monthly healthcare regulatory compliance updates. Compliance Updates: April 2024 Overlook: Licensure Compacts Other Legislation Board Updates Interstate Medical...

Give your customers the best data, analytics, user-friendly platforms, and the most comprehensive solutions for their healthcare background screening needs.
Verisys is an industry leader in pre-hire screening

Data aggregators and background screeners partner with Verisys to access FACIS® and other data sets to ensure their healthcare clients remain compliant.
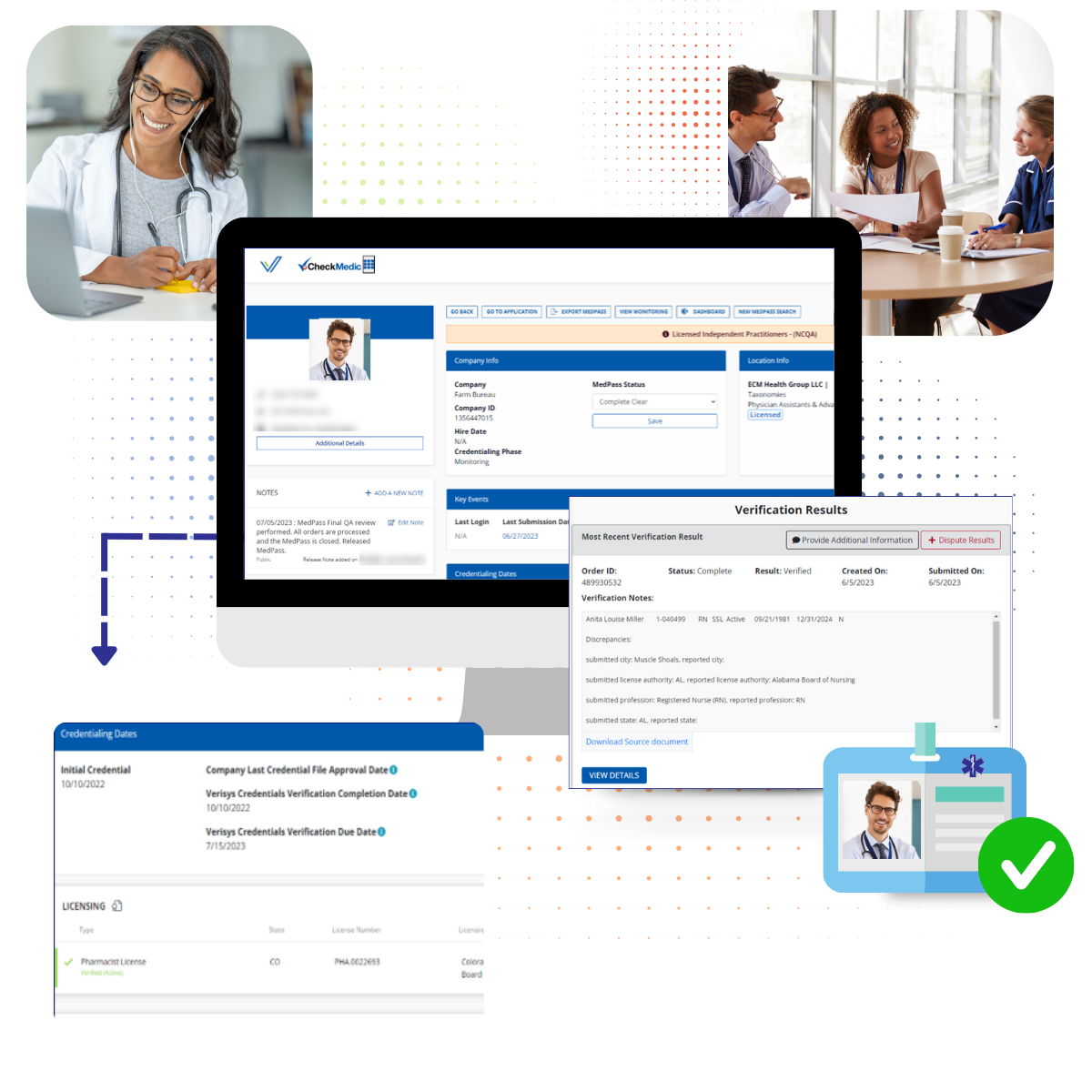
With Verisys, clients get 100% primary-sourced data delivered via our intuitive dashboard or digital delivery within an integrated partner platform. Whether your healthcare data clients need verifications and references for one individual or a hundred thousand, our results are accurate, consistent, and timely.
Quality Data with Flexible Access
We do more than provide verified data for background screening clients or data aggregators, we monitor any data points your clients need to track.
Accessing high-quality data, screening, and monitoring provide you with the most comprehensive software services and solutions for your clients.
Maintaining compliance and safeguarding against fraud and abuse in today’s changing healthcare landscape can be challenging.
Organizations that receive funds from Medicare, Medicaid, TRICARE, or other federal programs cannot afford to employ individuals or entities excluded from even one government program. Excluded from one means excluded from all, and the fines for non-compliance will likely be in the hundreds of thousands.
18 of the Top 20 U.S. background screeners choose Verisys to get the highest quality data for their clients.
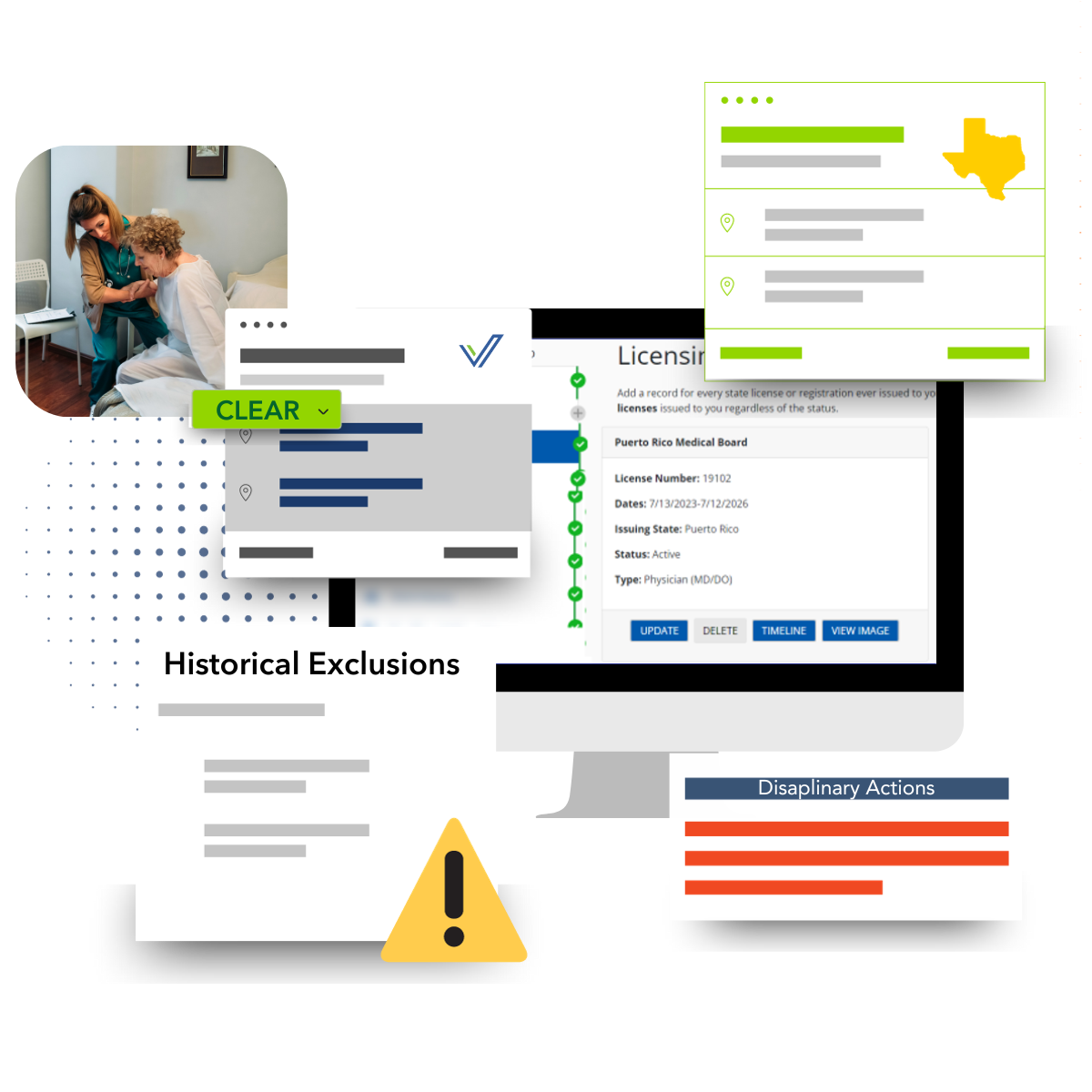
FACIS® is the Gold Standard in sanction and disciplinary action screening in the healthcare industry.

Verisys verifies professional license numbers, statuses, issue and expiration dates, and any current or historical disciplinary actions.

By validating an NPI number during the process of screening and monitoring providers for credentialing and enrollment, as well as referring supplier entities, you gain a valuable tool for complete transparency.

Avoid patient risk as well as brand and reputational risk when prescreening and monitoring for abuse.

Verification of DEA registration which allows providers to write prescriptions for controlled substance.

Detect fraudulent providers and identify invalid SSNs and misappropriation of identity.

Verisys’ OFAC+, a proprietary aggregated dataset, provides data related to anti-money laundering screening, a requirement under various federal laws and regulations.

Controlled Drug Substance (CDS) monitoring of providers is essential to prevent controlled substance fraud and abuse that could endanger patients.

Monitor FACIS® data, licenses, for status changes in licenses such as inactive, suspended, expired, or near expiration.