– The best resource for monthly healthcare regulatory compliance updates. Compliance Updates: April 2024 Overlook: Licensure Compacts Other Legislation Board Updates Interstate Medical...

FACIS® Data Supersource
FACIS® is a database of 10 million records from over 3,500 primary sources on provider exclusions, sanctions, and adverse events. Thousands of organizations rely on FACIS® to keep their customers safe. When it comes to keeping customers and patients safe, you need the gold standard.


Verisys FACIS (Fraud Abuse Control Information System) delivers 360-degree transparency on providers, staff, and entities for the organizations who hire, credential, refer, and reimburse for healthcare delivery such as retail pharmacies, telemedicine, staffing companies, health systems, payers, and pharmaceutical companies.
FACIS is the industry’s most comprehensive database consisting of primary content from federal and state sources for exclusions, sanctions, debarments, disciplinary actions, and adverse events against healthcare professionals and entities for all 868 taxonomies and all 56 U.S. states and jurisdictions.

Using FACIS makes it easy to maintain regulatory compliance by identifying red-flag behaviors and trends for any individual you employ.
With FACIS, organizations of any size can discover their true potential.

Here’s how FACIS® delivers value at every stage of your provider data management process:

Verisys performs verification matches on all possible matches to determine “true identity.” That means our team of verification analysts, who are specially trained to resolve false positives, verify matches using primary source data. Searching ALL aliases provided on each practitioner. This is a standard in our search criteria and verification process.
Faster verifications to accelerate efficiency and reduce fraud and waste.
FACIS® is the industry’s most comprehensive database consisting of primary content from federal and state sources for exclusions, sanctions, debarments, disciplinary actions, and adverse events against healthcare professionals and entities for all 868 taxonomies and all 56 U.S. states and jurisdictions. A database of over 10 million records from over 3,500 primary sources on provider exclusions, sanctions, and adverse events, FACIS® delivers 360-degree transparency on providers, staff, and entities for the organizations who hire, credential, refer, and reimburse for healthcare delivery.
When it comes to keeping customers and patients safe, you need the gold standard.

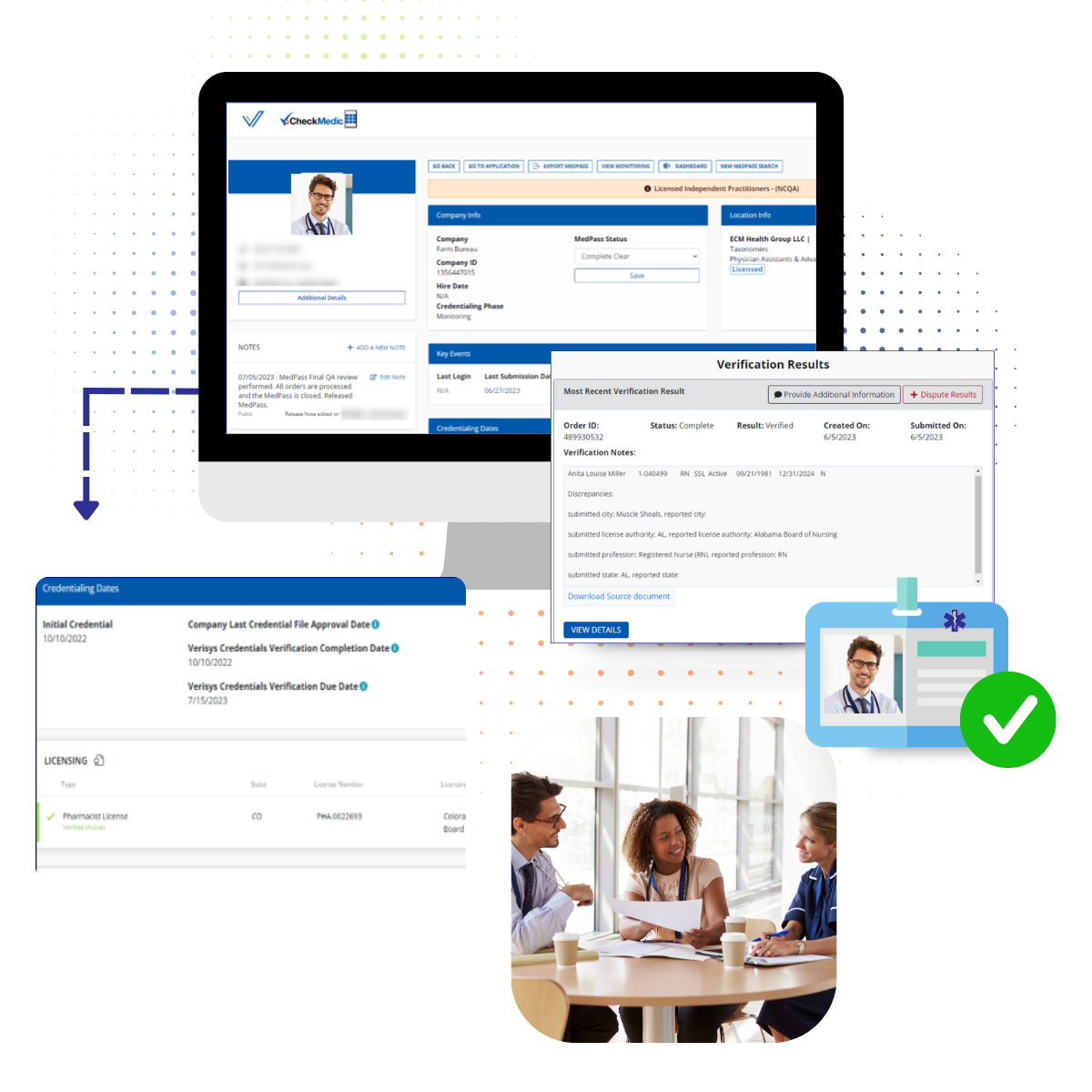
Continuously monitoring your population adds a layer of security and makes ongoing compliance with regulations set by standard-setting bodies possible. To stay in compliance with federal and state regulations and to keep patients safe, it’s vital for hospitals and health systems to monitor the licenses of their practitioners for new information that may prevent a physician from practicing. If a practitioner’s license is invalid, suspended, or expired, or if restrictions are placed on a license, healthcare organizations must take steps to halt the treatment of patients until the practitioner gets his license back in good standing.
The best way to ensure all practitioner licenses remain in good standing is through continuous healthcare license monitoring.
Every Data Set You Need
Assuring quality care to your patients and safeguarding your organization from fraud, waste, and abuse starts with data. Lots of data. FACIS draws from thousands of sources to give you maximum protection:

8,000,000+
Providers Monitored Annually
3,500
Primary Sources
2,200,000+
Credentialing Events Annually
What are partners are saying:
Learn more about what FACIS® can do for your organization
– The best resource for monthly healthcare regulatory compliance updates. Compliance Updates: April 2024 Overlook:...
March 2024 Bad Actor Roundup By Verisys Each month we will give a roundup of recent healthcare fraudsters and complia...
February 2024 Bad Actor Roundup By Verisys Each month we will give a roundup of recent healthcare fraudsters and comp...
As the healthcare industry is increasingly targeted for data theft and fraud, information security has emerged as a t...
Learn about Human Capital Management here. Verisys stands at the forefront of enhancing Human Capital Management (HCM...
At the core, Human Capital Management (HCM) within the healthcare sector focuses on the pivotal role of managing an o...