Verisys Eligibility: Where Accuracy Meets Assurance.
The Verisys Eligibility dataset is the Highest Quality & Most Accurate Transactional Data in the Industry
Retail Pharmacies
Health Providers
Government
Life Science
Health Plans
Pharmacy Benefit Management
Eligibility is designed to reduce organizational risk and improve operations for healthcare organizations.

Manage Risks With Unmatched Visibility
- Pre-Enrollment screening to ensure a provider is eligible to see patients.
- Point of prescription fill eligibility screening to ensure your eligibility to provide medicine.
- Eligibility screening at point of claim payment to help reduce fraud, waste, and abuse.
- Underwriting risk assessment for providers and entities

- Real-time confirmation of prescription fills and immediate alerts to changes in status.
- Real-time review of prescribing provider status and alerts to potential issues
- Real-time transactional pre-employment screening
- Verify providers hold the required licenses and maintain a clean record.
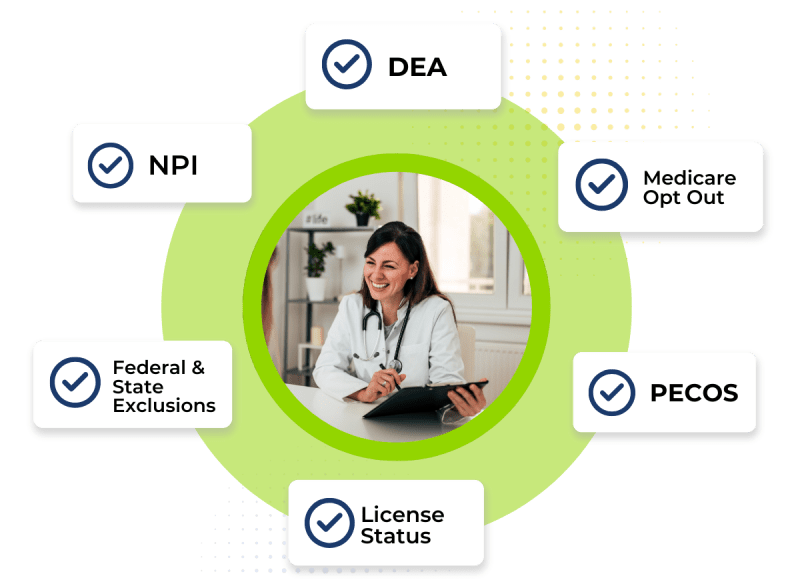
Screen against state & federal exclusions, NPI, license status, DEA, PECOS, and medicare opt out


- Real-time confirmation of eligibility for pre-enrollment screening
- Real-time confirmation of eligibility screen at point of claim payment
- Real-time review of underwriting risk assessment
- Real-time transactional pre-employment screening
- Real-time review of prescribing provider status and alerts to potential issues


- Real-time confirmation of eligibility for pre-enrollment screening
- Automated credential verification
- Promptly confirm licensure and/or certification for relevant positions
Ensuring qualified candidates are swiftly onboarded, minimizing administrative burdens, and fostering a seamless recruitment experience.
%
of Individuals Submitted are Identified
Providers Monitored Annually
%
Verification Accuracy

- Seamless API integration into existing organizational tech stack to streamline reporting
- Pre-schedule eligibility screening to minimize potential missed screenings
- Minimize the need for additional data to be provided from your organization


FACIS®

License Verification

Pre to Post Hire Screening

Workforce Management















