Optimized Healthcare Credentialing
Powered by Verisys
Our services ensure the highest standards in healthcare credentialing by streamlining the provider credentialing process. Whether you’re verifying healthcare providers, managing physician credentialing, or handling provider enrollment, Verisys offers tailored solutions to meet your organization’s requirements. With industry-leading tools, we optimize the credentialing process, reduce costs, and improve operational efficiency, enabling healthcare professionals to focus on patient care.

Streamlined Credentialing - Powered by Verisys
Experience superior credentialing solutions backed by decades of expertise. Our process ensures medical credentialing accuracy, tracks board certifications, and meets compliance standards for all healthcare organizations. Simplify credentialing while delivering unmatched precision and speed. Trust Verisys to verify qualifications, ensure proper privileges, and streamline your hospital or healthcare facility operations.
Why Verisys?
Because Accuracy and Speed Matter.
Delays in credentialing healthcare professionals can impact patients and revenue. Verisys minimizes inefficiencies through verified data, accurate verification processes, and seamless integration with insurance and health plans. Here’s why Verisys is your trusted partner:
Golden Record Credentialing Dataset
- Achieve faster, more accurate credentialing with Verisys’ continuously updated, verified provider information and data. With every status change tracked, you’ll always have the latest information.
- Verified primary source data attached to a provider’s profile to improve approval and turnaround time. Provider data is continuously re-confirmed and updated based on status changes. Data aligns with clinical, payer, and licensure standards.


All Taxonomies. All Provider Types.
Our comprehensive approach means no credentialing need is too big or too complex.
- Verisys data drives credentialing for all taxonomies and all provider types.
- Verisys handles common credentialing standards such as NCQA, URAC, TJC, and more. It also handles all provider types, including MDs, RNs, Allied Professionals, and more.
Credentialing That Works For You
- Whether supporting in-house teams or taking on your full credentialing operations, Verisys delivers. We improve turnaround times, reduce manual effort, and get providers network-ready faster than ever.
- In-house teams can access the same information the Verisys team utilizes for primary source verification.
WHAT WE DO
Credentialing Operations Optimized
Efficient and Scalable Solutions:
Whether you’re a small health plan or a large healthcare system, our credentialing services are scalable to meet your needs, allowing you to focus on what matters most—patient care. Our solutions are designed to reduce the administrative burden on your staff while ensuring that all providers are credentialed to the highest standards.
Accelerate Time to Treat Patients:
Verisys significantly shortens the credentialing process, enabling providers to start treating patients sooner and thus boosting health systems’ revenue opportunities.


Verisys allows your team to focus on what they do best
while we handle the complexities of credentialing with unmatched speed, efficiency, and quality.
OUR STATS
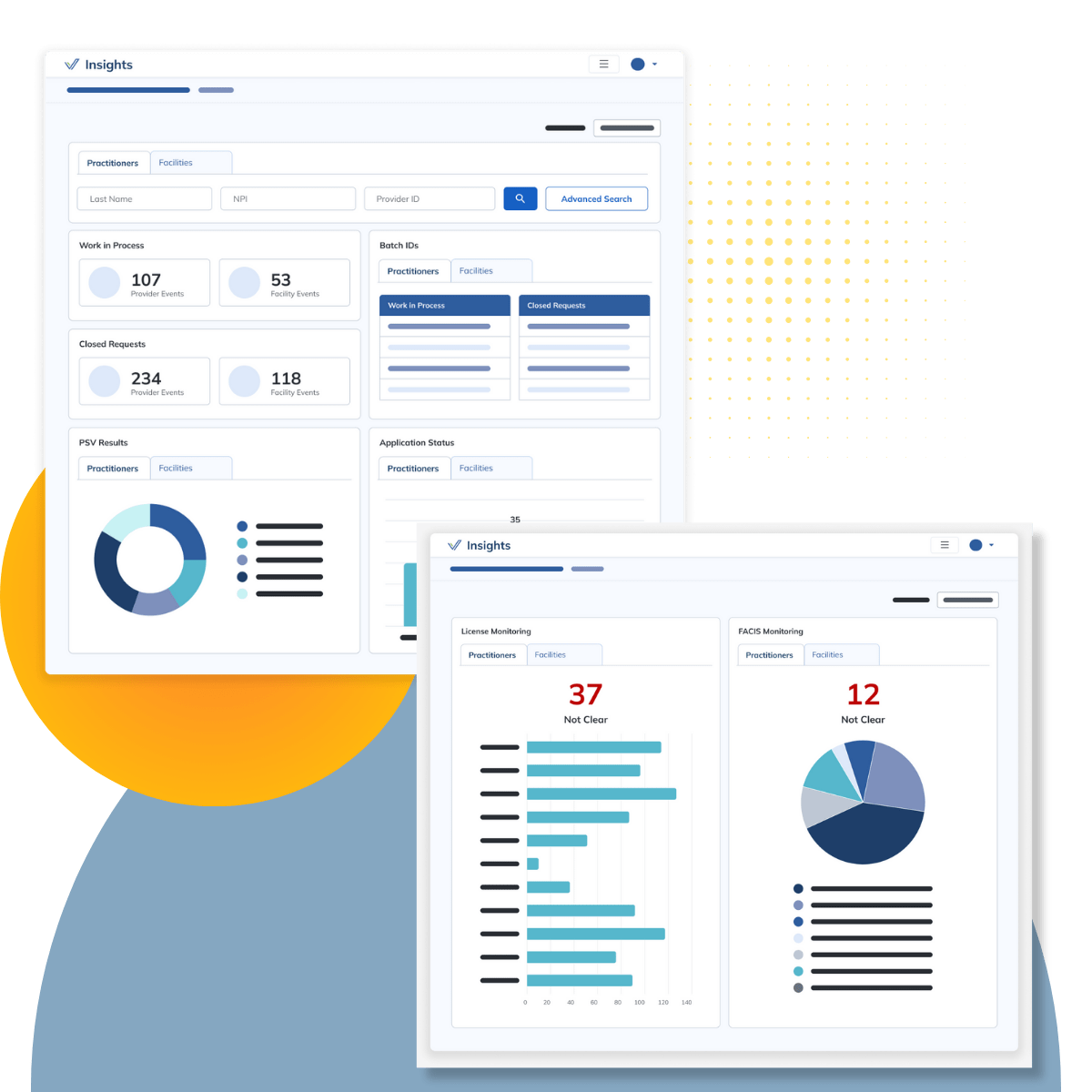
The Stats That Matter
Serving the largest and most complex healthcare organizations for over 30 years, Verisys is the leader in credentialing solutions. With over two million events annually, our provider credentialing services provide exceptional accuracy while accelerating speed to network to deliver exceptional outcomes.

Credentialing Events Annually

Annual Screening Searches

Providers Monitoring Annually

Primary Sources
3 Ways Verisys Optimizes Credentialing
01
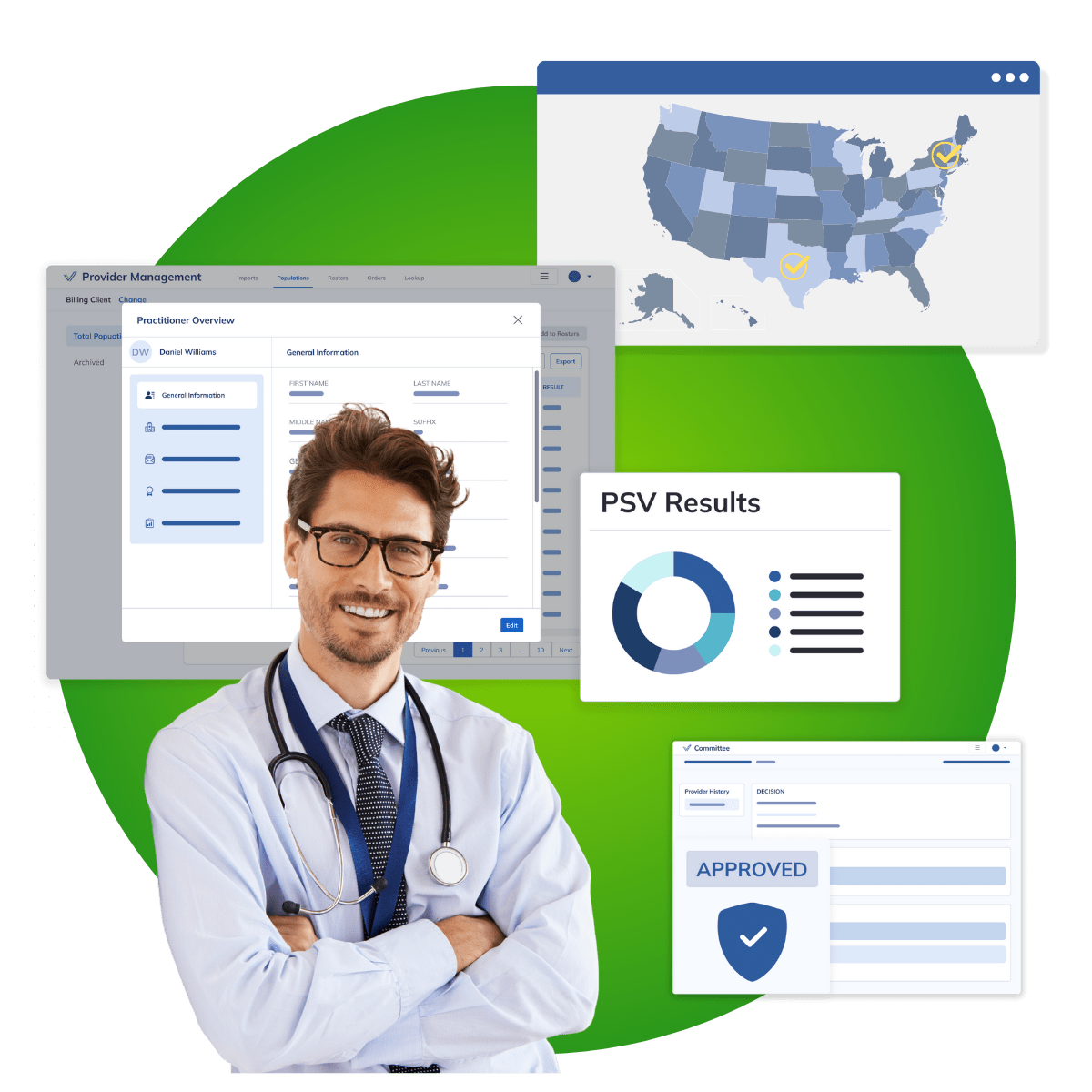
In-House Credentialing Powered By Verisys
Support in-house credentialing teams with Verisys data to streamline the credentialing process and reduce turnaround times. Utilize Verisys Verified data to confirm healthcare provider information. Verisys facilitates over 2 million annual outsourced medical credentialing events, ensuring accuracy and compliance.

02
Outsourced Credentialing to the Best
Outsource some or all aspects of provider credentialing to Verisys. As the largest CVO, we handle even the most complex credentialing healthcare demands and manage high volumes of credentialing events with precision and reliability.
03
Full Suite, Full Control
Verisys supports all aspects of the provider credentialing process from network invites and application gathering to primary source verification, committee review, and recredentialing. Our full-suite solutions are designed to meet the specific requirements of your healthcare facility or organization, empowering compliance and operational efficiency.
How Verisys Optimizes Credentialing
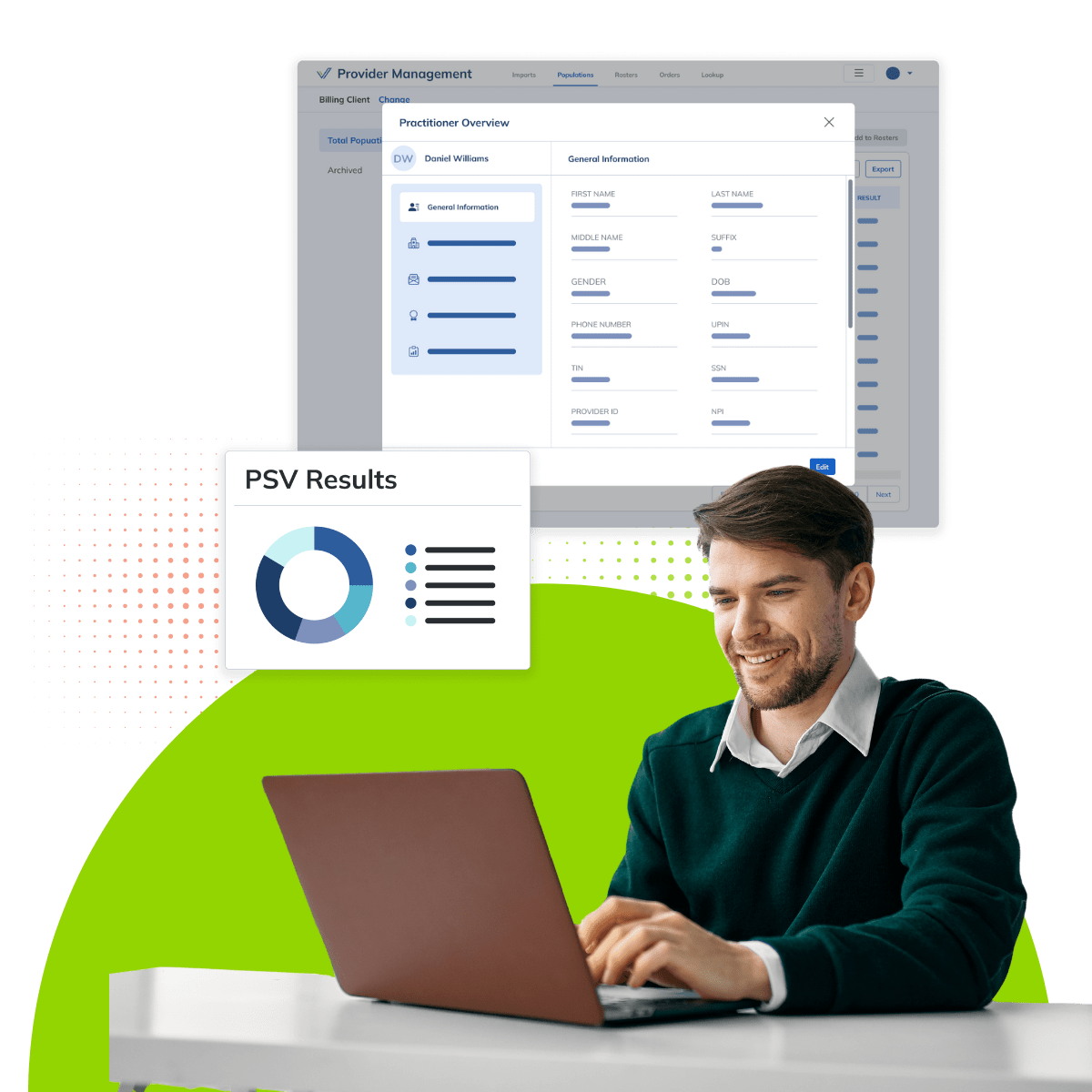
The Process:
Data Curation
We collect and curate pristine datasets, powering healthcare compliance and credentialing solutions.
Proprietary Matching & Verification
Through expert data matching and verification, Verisys creates comprehensive provider profiles, achieving a 99.9% accuracy rate. This ensures your healthcare professionals meet the highest standards of quality and competency.
Real-Time Monitoring
Continuous monitoring powered by Verisys ensures healthcare credentialing compliance in real-time.
Compliance Optimization
Implement Verisys data to enhance and streamline your compliance programs.

WHAT WE DO
Better Data, Better Decisions, Better Outcomes – Powered by Verisys
Our medical credentialing services cover all aspects of healthcare provider verification, from primary source verification to ongoing monitoring, and supporting practitioner compliance. With Verisys, you can trust that your providers are thoroughly vetted and compliant with industry standards, ultimately enhancing patient safety.
Verisys provides industry-leading primary source verification services, giving you peace of mind that your healthcare providers’ credentials are accurately and independently verified at the source, helping to maintain compliance with industry standards.
Credentialing Built to Meet the Highest Standards
No matter which credentialing standards you follow, Verisys is equipped to meet them with precision. From NCQA to The Joint Commission, our expertise ensures your organization stays compliant and ahead of the curve.
NCQA Credentialing
NCQA credentialing standards are the most common standards utilized. Verisys is an NCQA accredited CVO. Our data helps your organization meet NCQA standards.

NCQA Credentialing and Recredentialing
As an NCQA-accredited CVO, Verisys helps you achieve and maintain NCQA credentialing standards, ensuring compliance with the strictest requirements.

URAC Credentialing
Verisys delivers solutions that meet URAC standards, helping your organization maintain oversight and accountability in every credentialing step.

The Joint Commission Credentialing
We support organizations in meeting The Joint Commission’s credentialing requirements, providing a comprehensive approach to compliance.
Frequently Asked Questions: Your Credentialing Questions, Answered
Still have questions? We’ve got you covered. Check out the answers to our most commonly asked questions regarding our credentialing solutions below.
Other Questions?
Reach out to our team to learn more about our credentialing offerings. Contact us here.
What credentialing solutions does Verisys offer?
Verisys offers several credentialing solutions including provider credentialing data to support in-house teams, hybrid workflows, and fully outsourced medical credentialing services.
What standards and provider types can you credential?
We credential all healthcare provider types and adhere to any standard, including NCQA, URAC, and The Joint Commission. Verisys handles credentialing of all sizes and complexities, meeting the diverse needs of healthcare organizations.
What are your organization's certifications + accreditations?
Verisys is certified and accredited by both NCQA and URAC. We are the only credential verification organization that has both qualifications.
What is your relationship to CAQH?
Verisys is partnered with CAQH to integrate the CAQH application into the Verisys workflow to streamline the application process. Beyond this application integration, Verisys and CAQH have partnered together to streamline credentialing solutions. To learn more, please contact sales@verisys.com.
Ready to Elevate Your Compliance?
Contact us today to learn more about Verisys healthcare compliance solutions and how we can integrate our Gold Standard data to meet your unique needs.
Your Compliance Data Partner
Expand Your Compliance Capabilities with These Essential Datasets
Verisys goes beyond credentialing, offering additional datasets to support your organization’s broader compliance and credentialing needs.

License Verification & Monitoring
Continuous monitoring of provider licenses to ensure compliance.
DEA, CDS, Abuse Registry, OFAC+
Streamline your compliance checks with access to critical databases and records.
















