PECOS enrollment determines whether your organization can participate in Medicare, receive reimbursement for services, and maintain compliance with federal and state healthcare regulations. Yet many healthcare providers struggle with enrollment delays, application denials, and data mismatches that disrupt revenue cycles and patient care access.
This guide explains what PECOS is, how the enrollment process works, and the common challenges that create bottlenecks in Medicare participation. You’ll learn practical ways to manage enrollment more effectively, maintain accurate provider data across systems, and reduce the errors that trigger development requests and payment holds.
What Is PECOS?
PECOS is the Provider Enrollment, Chain, and Ownership System: Medicare’s online Medicare enrollment management system. It allows healthcare providers to enroll in the Medicare program, update their enrollment information, and manage participation status electronically. PECOS replaced paper-based CMS-855 enrollment forms, enabling Medicare Administrative Contractors to process enrollment applications more efficiently.
Physicians, nurse practitioners, hospitals, group practices, and medical equipment suppliers all use PECOS to manage enrollment and obtain PTANs required for Medicare billing. For most organizations, PECOS serves as the primary gateway to Medicare participation and reimbursement.
Why PECOS Enrollment Is Important for Healthcare Providers
Your PECOS enrollment status directly determines whether you can bill Medicare and receive payment for services. Without proper enrollment, claims are denied, leaving organizations unpaid for care already delivered. Lost provider capacity often translates into unrecoverable revenue¹, particularly when plan-year deductibles reset and appointment slots go unfilled.
Accurate PECOS data also supports compliance with CMS regulations. Incomplete or outdated data can trigger a hold on your Medicare reimbursement or deactivation of billing privileges, affecting your revenue and patient care operations. Enrollment issues may also limit a provider’s ability to order, certify, or prescribe services for Medicare beneficiaries.
Identifying potential issues early by performing healthcare exclusion screening helps you address problems before they result in enrollment complications or penalties.
How PECOS Enrollment Works
The PECOS system manages your entire Medicare enrollment lifecycle through a secure online portal, covering everything from initial applications to regular revalidation and ongoing updates to your practice information.
Digital Enrollment and Revalidation
You submit your initial enrollment application electronically through the PECOS portal, where data is validated in real time. This validation reduces processing delays compared to traditional paper submissions.
Medicare requires providers to revalidate every five years to confirm that all provider information remains current and accurate, though DMEPOS suppliers must revalidate every three years. During this process, you must electronically sign and submit supporting documents, including license and ownership information.
Verifying that your licensure data matches primary sources, such as through healthcare license verification, can help reduce development requests and speed approval times.
Managing Ownership and Practice Information
PECOS requires detailed ownership, organizational structure, and practice location disclosures to meet federal requirements. Changes to this information must be reported promptly to maintain enrollment status.
Accurate affiliations, taxonomy codes, and reassignment details are critical to avoid enrollment denials. Performing exclusion screening before you submit your PECOS application helps prevent compliance flags by identifying sanctions or exclusions ahead of a MAC review.
PECOS Identity & Access Setup
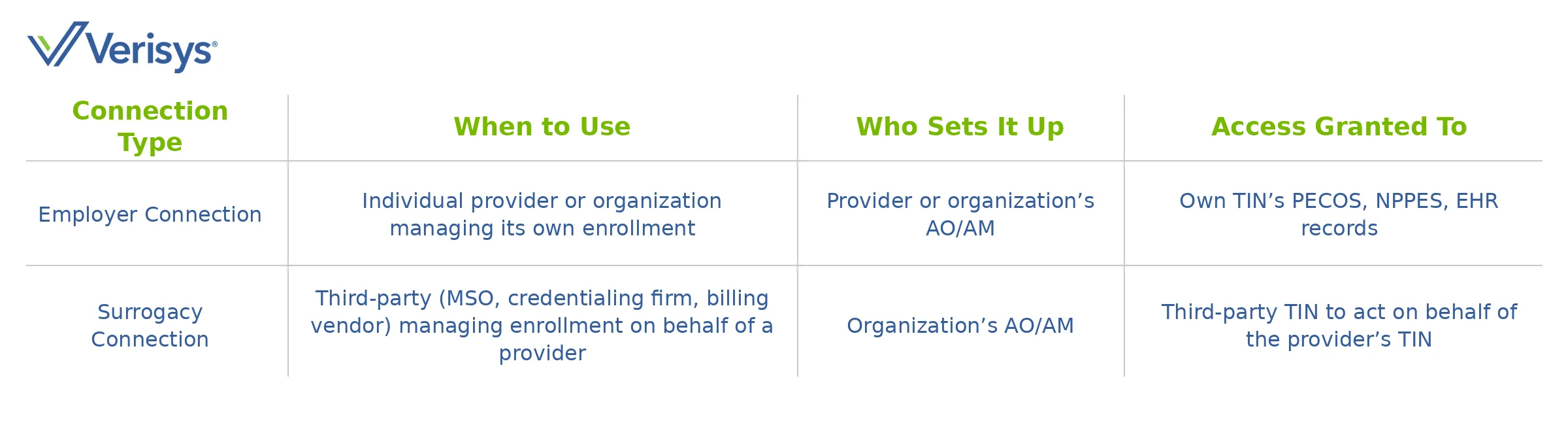
The Identity & Access Management system controls who can access PECOS and other CMS systems, requiring proper setup before you can manage your enrollment. Two connection types allow different levels of access:
- Employer connections, which link individuals to their own organization’s records
- Surrogacy connections, which allow third parties to manage enrollment on a provider’s behalf
Key roles include the Authorized Official who signs applications and the Access Manager who controls system access. Common setup problems that delay enrollment include:
- Authority mismatches – The designated AO lacks legal authority to sign for the organization
- Missing surrogacy – Third parties forget to complete surrogacy requests before starting applications
- Lost credentials – Forgotten passwords lock users out and delay submissions
 Common PECOS Enrollment Challenges
Common PECOS Enrollment Challenges
Many providers face similar problems that delay or deny their PECOS enrollment, but understanding these issues helps you avoid them and submit successful applications. With healthcare facing a $20 billion opportunity to reduce administrative waste, accurate enrollment processes become even more critical.
Common challenges include:
- Mismatched legal names or tax identification numbers
- Outdated NPI or licensing data
- Missing or expired licenses
- Complex ownership structures that trigger development requests
Complex ownership structures often create confusion and trigger development requests from Medicare Administrative Contractors, highlighting the importance of maintaining provider data accuracy across all systems.
When information does not align across PECOS, NPPES, licensing boards, and IRS records, processing timelines can extend significantly. Using healthcare provider data verification solutions helps ensure consistency before submission.
Additionally, missing electronic signatures or unsigned certification statements within the required timeframe will result in automatic application rejection.
Best Practices for Using PECOS Effectively
Smart PECOS management starts with organizing your provider data and coordinating across your teams to prevent errors and keep your enrollment up to date.
Since CMS posts revalidation due dates seven months in advance, you have ample time to prepare when you implement proper tracking systems. Credentialing solutions can support these efforts by centralizing data and automating validation workflows.
Focus on these key actions to streamline your PECOS management:
- Centralize provider data – Create a single source of truth for identity, licensure, sanctions, and practice information
- Automate alerts – Set reminders for revalidation dates, license expirations, and required updates
- Pre-submission checks – Implement provider data validation against primary sources before submitting to avoid development requests
- Define roles clearly – Document who can sign applications and manage surrogacy connections
PECOS Enrollment as a Core Tool for Medicare Compliance
PECOS enrollment plays a critical role in Medicare participation, reimbursement protection, and regulatory compliance. Accurate, verified provider data helps prevent enrollment delays, claim denials, and billing interruptions that can affect both revenue and patient access to care.
Verisys provides real-time, verified data solutions that help healthcare organizations manage PECOS enrollment with confidence. By leveraging pristine, curated, and monitored datasets, you can automate critical verification processes, reduce administrative burden, and ensure your provider information meets regulatory standards.
Sources
- CAQH. The CAQH Index Report. https://www.caqh.org/insights/caqh-index-report
- Centers for Medicare & Medicaid Services (CMS). Revalidations (Renewing Your Enrollment). https://www.cms.gov/medicare/enrollment-renewal/providers-suppliers/revalidations


 Common PECOS Enrollment Challenges
Common PECOS Enrollment Challenges



















