Patients want optimum healthcare and are willing to sue if they get anything short of that. Regulatory bodies also have a high standard for healthcare providers and professionals. Digital healthcare and telemedicine have brought even more risk to the picture.
The stakes are high, and you need guidance to navigate today’s biggest legal issues in healthcare. Let’s guide you.
Overview of Current Healthcare Legal Challenges
Healthcare is one of the most heavily regulated industries in the United States. Providers, payers, hospitals, and health systems must operate under a complex web of federal, state, and local laws, all while delivering care, protecting patient data, and billing accurately.
There are five primary risk areas for legal issues in hospital administration:
- Data privacy and security
- Fraud, waste, and abuse (FWA)
- Telehealth regulation
- Malpractice and liability
- Regulatory compliance across jurisdictions
Failure in any of these areas can result in severe penalties, including loss of licensure, exclusion from federal programs, class-action lawsuits, and even huge fines.
In fact, in 2023, the U.S. Department of Health and Human Services (HHS) Office for Civil Rights (OCR) imposed $68,928 in HIPAA penalties for each willful privacy violation that remains uncorrected.
A proactive legal strategy, supported by strong compliance frameworks and real-time data visibility with healthcare provider data verification solutions, is no longer optional. It’s essential for risk mitigation and long-term operational viability.
Data Privacy and HIPAA Compliance
The Health Insurance Portability and Accountability Act (HIPAA) mandates strict privacy and security standards for the handling of Protected Health Information (PHI). Covered entities, including providers, payers, and business associates, must implement physical, administrative, and technical safeguards to prevent unauthorized access or disclosure.
With the rise of electronic health records (EHRs), patient data now moves across more systems and platforms than ever before. However, many EHR vendors lack encryption safeguards, exposing providers to third-party risk.
Healthcare organizations must conduct regular HIPAA security risk assessments, access audits to detect unauthorized viewing, perform vendor due diligence, and evaluate cybersecurity insurance.
Fraud, Waste, and Abuse Prevention
Fraud, waste, and abuse in healthcare cost the U.S. government billions of dollars annually. This includes billing for services not rendered, upcoding procedures, unbundling charges, kickbacks, or illegal referrals.
Federal and state programs, including Medicare, and Medicaid have intensified audit efforts. These audits often result in payment recoupments, civil monetary penalties, and criminal referrals to the DOJ or FBI.
Preventing fraud requires a culture of compliance backed by real-time billing oversight, credentialing accuracy using healthcare provider credentialing solutions, and thorough internal healthcare audits.
Telehealth Legal and Regulatory Issues
Telehealth exploded after the pandemic in 2020, and the related legal issues have kept increasing since then.
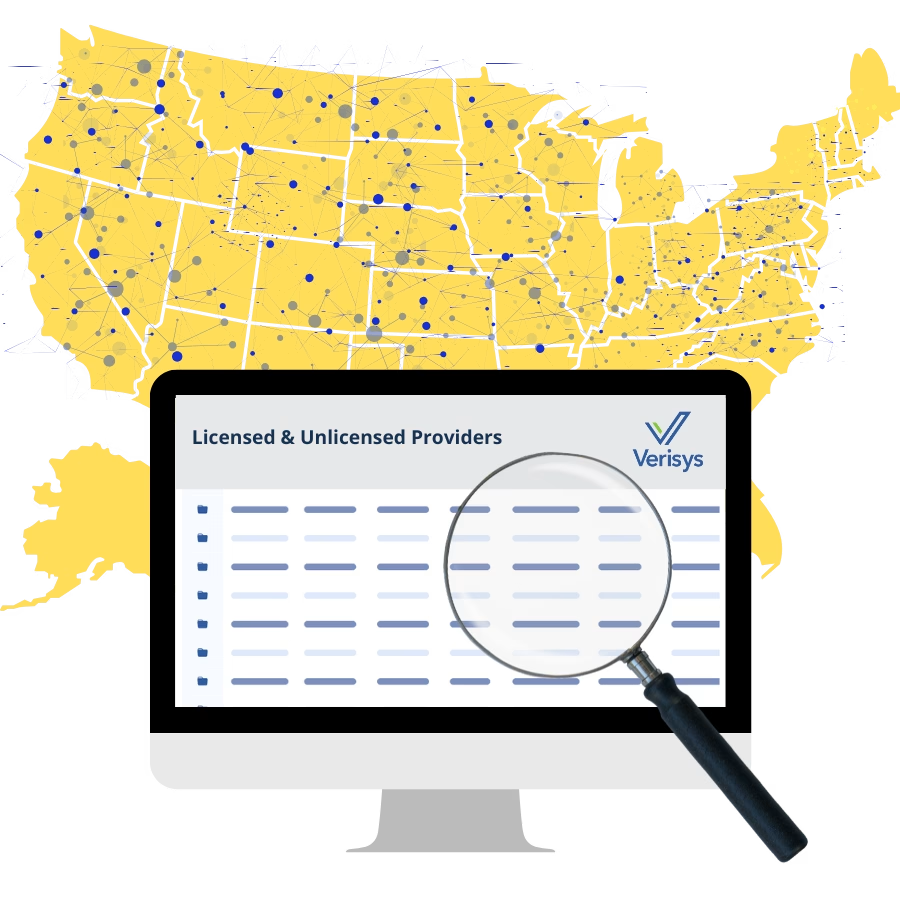
One major challenge is licensing. Most states require providers to be licensed where the patient is located, not just where the clinician practices. Providers offering telehealth across state lines must secure and maintain multiple state licenses, each with its requirements.
The Interstate Medical Licensure Compact (IMLC) covers physicians in 40 states currently, so practicing in the other states will often require more complex, state-specific hurdles. Practicing without proper licensure can trigger penalties, audits, and reimbursement denials.
Getting paid for telehealth is also tricky. Medicare covers some virtual visits but has strict rules, like where the patient is located and whether the visit is video or audio-only.
Privacy is another big concern. Telehealth still has to follow HIPAA laws that protect patient information.
Other Emerging Legal Concerns
There’s more to look out for with each passing day. Here are a few legal concerns you should keep an eye out for:
1. Medical Malpractice
Rising patient awareness, evolving standards of care, and digital record-keeping have increased exposure. Legal concerns include missed diagnosis, delayed care, and negligent credentialing of providers with disciplinary history.
Accurate provider credentialing is now a core defense strategy. Systems like Verisys help vet provider backgrounds, sanctions, and licensure in real time, minimizing risks.
2. Regulatory and Policy Shifts
Healthcare regulations shift frequently. Recent healthcare law cases involve increased expectations in price transparency, cybersecurity, and provider background screening.
Failure to keep pace with state and federal changes, especially during mergers or acquisitions, can lead to lawsuits, delays in payer onboarding, or licensure issues.
Best Practices for Legal Risk Management
You can manage the healthcare legal risks to ensure that legal issues are minimal or even non-existent in your practice or facility. Here are a few things to put in place:
1. Build a Compliance-First Culture
There’s never enough training on legal issues. There should be ongoing HIPAA and FWA training for all teams, and incident response SOPs should be documented and within reach for all staff.
There should also be frequent internal audits of billing access logs. These programs should be updated annually to reflect changes in the law and internal operations.
2. Integrate Legal Counsel Early
Legal counsel should be involved from the start, not just when problems arise. A legal advisor should be involved in reviewing payer contracts and enrollment documents, overseeing provider onboarding and credentialing, and advising on scope-of-practice issues, especially for multi-state clinicians.
General counsel should work closely with the compliance, credentialing, and revenue cycle teams to ensure unified risk oversight.
Staying Ahead of Legal Issues
Healthcare is becoming complex, digital, and more regulated. From data privacy enforcement to telehealth licensing and fraud laws, the risks are growing, but so are the tools to manage them.
Organizations that take a proactive, structured approach to legal compliance, integrating real-time monitoring, regular training, and automated credentialing, are better positioned to avoid penalties, protect patients, and stay ahead of costly disruptions.
Verisys helps prevent credentialing-related malpractice and compliance issues with integrated healthcare credentialing and provider compliance solutions that surface risks early.
Sources
IMLC: Pathway to physician licensure
https://imlcc.com/a-faster-pathway-to-physician-licensure/
Sullivan Benefits: Penalties for HIPAA Violations Increase