Choosing the right credentialing verification vendor directly affects whether your healthcare organization can maintain compliance, protect patient safety, and operate efficiently. This is especially important when credentialing fails, organizations face delays in onboarding, missed exclusions, audit exposure, and legal and financial risk.
The vendor you select directly impacts your ability to verify provider credentials accurately, monitor sanctions in real time, and protect patients from unqualified or excluded providers.
This complete guide explains what to look for in a credentialing partner or verification vendor and outlines the key factors to consider when choosing a credentialing service provider. Here, we will focus on accuracy, regulatory adherence, automation, and scalability within the credentialing process, helping healthcare leaders select the right credentialing service provider to support long-term operational performance.
Why Choosing the Right Credentialing Vendor Matters
In the healthcare industry, vendor credentialing is the process of validating that individuals and companies meet required standards before they can access facilities, systems, or patients. The vendor credentialing process supports safe and effective patient care by confirming licenses and certifications, conducting background checks, validating qualifications, and verifying adherence to laws and regulations that underpin vendor credentialing compliance.
At a minimum, the credentialing process ensures that vendors and providers meet specific requirements, including:
- Valid licenses and certifications
- Appropriate qualifications and training
- Completed background checks
- Proof of liability insurance
- Adherence to laws and regulations
For healthcare facilities, this process is critical in healthcare operations and directly supports healthcare compliance audit preparation by ensuring documentation, monitoring, and verification are consistently maintained. Credentialing ensures that only qualified vendors can provide goods and services, particularly when they require access to sensitive systems, clinical spaces, or patient information.
When credentialing is handled poorly, provider onboarding gets delayed and healthcare organizations face compliance risks that can result in regulatory penalties from the OIG, CMS, and state boards.
Additionally, healthcare organizations must maintain strict oversight, as NCQA requires organizations to conduct monthly monitoring of sanctions, exclusions, and limitations¹.
Key Factors to Consider When Evaluating Credentialing Vendors
Selecting the right credentialing service provider requires careful evaluation of their expertise, technology, data quality, and scalability. These core factors ultimately determine whether your vendor can streamline operations while maintaining the compliance standards your organization requires.
Compliance Expertise and Regulatory Knowledge
Compliance is the foundation of any effective credentialing service.
Your credentialing service must demonstrate a deep understanding of regulatory requirements and the ability to apply those standards consistently across healthcare environments.
A credentialing service provider should be able to ensure compliance with oversight from key regulatory bodies, including:
- Office of Inspector General (OIG) exclusion lists
- Centers for Medicare and Medicaid Services (CMS) requirements
- National Practitioner Data Bank (NPDB) reporting
- State licensing boards and accrediting organizations
For hospital vendor access, credentialing must also account for vendor credentialing requirements that go beyond licensure. These often include:
- Verification of vendor credentials and qualifications
- Proof of liability insurance
- Completion of required training and education
- Ongoing OIG exclusion monitoring to support continuous compliance and protect the organization from regulatory penalties.
Effective credentialing solutions ensure that providers and vendors remain compliant over time, not just at onboarding. This level of oversight protects healthcare organizations from regulatory violations, supports audit readiness, and helps address any issues before they escalate.
Technology and Automation Capabilities
Modern credentialing relies on automation to reduce manual workload, minimize human error, and accelerate review cycles through dashboards, workflow tools, and automated alerts. In practice, credentialing involves coordinating data, documentation, and approvals across teams, systems, and external parties. What automation does is simplify these processes while improving efficiency and accuracy.
For healthcare organizations, the impact is material. The industry demonstrates significant cost savings potential, with $222 billion avoided² annually through automation initiatives that streamline the process of administrative work tied to credentialing, provider enrollment, and compliance oversight.
Your credentialing platforms should offer configurable workflows that adapt to different operational realities, including:
- Supporting healthcare systems, health plans, and specialty providers
- Managing vendor relationships and credentialing activities across state lines
- Maintaining audit readiness for a facility’s network
A modern portal also plays an important role by making credentialing data more transparent and easily accessible to internal teams and external partners.
Data Accuracy and Primary Source Verification Quality
Primary source verification validates a credentialing provider’s qualifications directly with issuing authorities, such as state boards and certification bodies. This step is essential for meeting standards and regulations, maintaining quality and compliance, and supporting strong data security across credentialing and provider enrollment workflows.
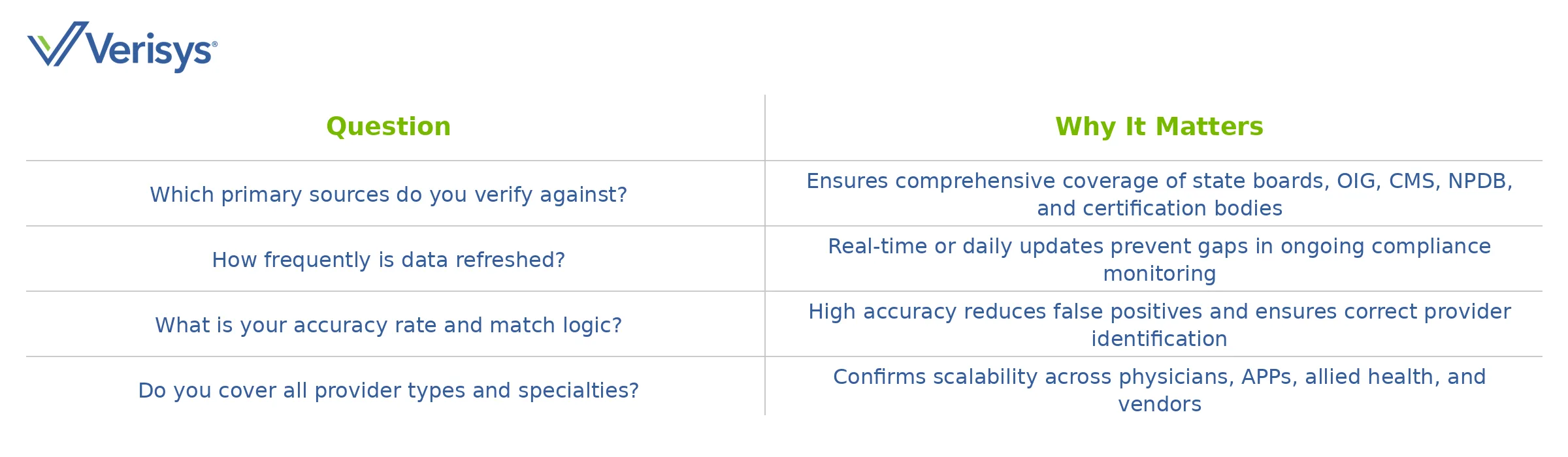
When evaluating a vendor’s methods, organizations should confirm what is required for vendor credentialing, including sources, refresh frequency, match logic, jurisdictional coverage, error rates, and how third-party data is validated and protected. Verification operates at a significant scale, with NPDB processing 12.5 million queries³ in 2023, making accuracy and infrastructure critical.
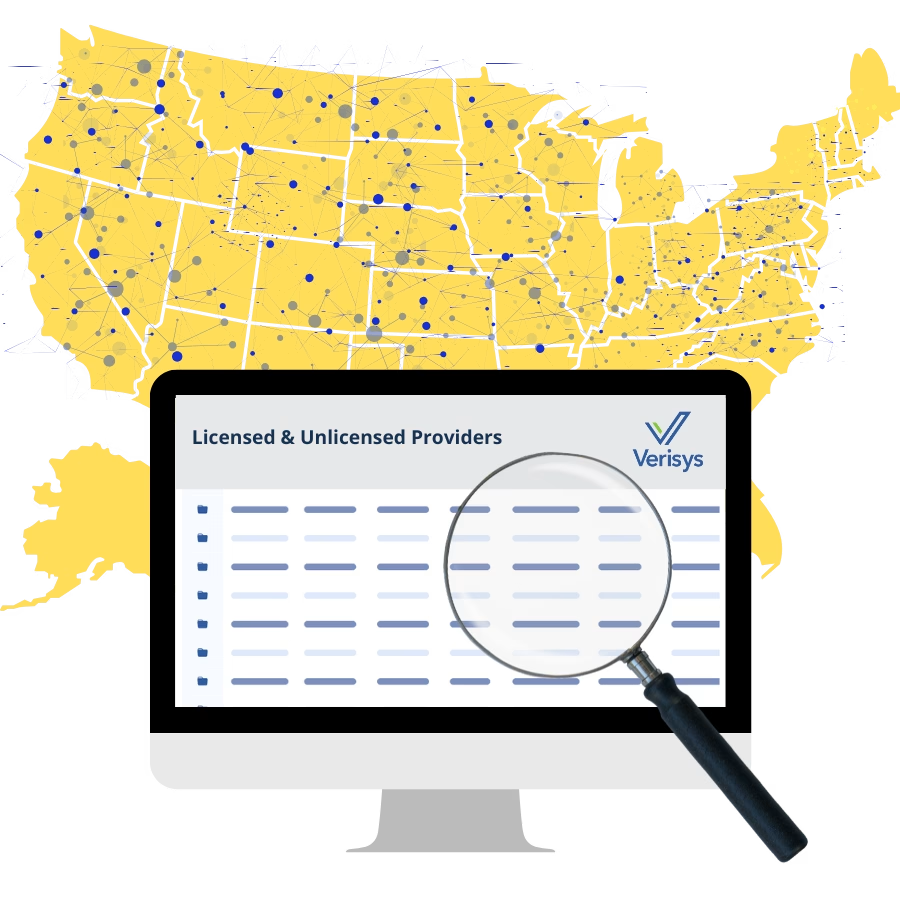
High-quality healthcare provider data verification solutions deliver real-time, verified data with proven accuracy by consolidating licensure, sanctions, and exclusions from primary sources.
Use these questions to evaluate verification quality:
Key Questions to Evaluate PSV Quality
Scalability and Customization
Credentialing workflows must adapt as organizations grow, whether supporting a single-site practice or a national health plan. In many organizations, vendor credentialing is typically managed separately from clinical credentialing, even though both rely on consistent data and oversight.
Scalable solutions should support:
- Multi-entity and delegated credentialing models
- Alignment with broader supply chain and network governance requirements
- State-specific rules, specialty requirements, and evolving vendor needs
The right vendor credentialing system helps organizations simplify expansion by ensuring vendors are qualified to provide services without disrupting care delivery or operations.
Customer Support and Service Reliability
Of course, technology alone isn’t enough. Strong customer support, onboarding assistance, and responsive account management are critical resources for healthcare organizations navigating complex credentialing requirements. Medical groups consistently emphasize the importance of holding vendors to written SLAs and defined turnaround targets⁴.
Organizations should ask about:
- Implementation timelines and onboarding support
- SLAs for uptime and request turnaround
- Escalation paths for urgent issues
Dedicated account managers and comprehensive training resources help with vendor credentialing, helping staff remain confident as requirements evolve.
Common Mistakes Healthcare Organizations Make When Choosing a Vendor
Selecting a credentialing partner without adequate due diligence can introduce legal, financial, and operational risk, including broader healthcare legal issues tied to improper access, billing, or compliance failures. Industry research continues to point to a $20 billion opportunity² to reduce waste through better credentialing and compliance processes.
Here are the most critical mistakes to avoid:
- Prioritizing cost over quality or compliance – Choosing the lowest-cost vendor credentialing service often leads to incomplete verification, missed exclusions, and audit failures that cost significantly more long-term.
- Overlooking integration requirements – Failing to evaluate how credentialing platforms integrate with existing systems creates duplicative work and fragmented data across departments.
- Failing to evaluate reporting capabilities – Lack of audit trails, performance tracking dashboards, and compliance reports limits visibility into vendor quality and regulatory adherence.
These missteps often affect credentialing organizations across both clinical and vendor domains, increasing exposure and slowing onboarding.
Questions to Ask When Comparing Credentialing Vendors
To discover what vendor credentialing capabilities truly support compliance, focus on questions that reveal data quality and operational maturity.
Ask how the platform validates data, how exclusions are monitored, and how updates are delivered to ensure that the provider remains eligible over time. Comprehensive healthcare exclusion screening provides monitoring across federal and state exclusion lists with continuous updates. Confirm alignment with NCQA, URAC, TJC, HIPAA requirements, and payer delegation rules.
Finally, request examples of audit-ready reports, compliance dashboards, expiration alerts, and performance metrics that streamline regulatory reviews. Automated healthcare license verification helps organizations maintain compliance without manual tracking, particularly for vendors and providers operating across state lines.
Choosing a Vendor That Strengthens Compliance and Efficiency
The right credentialing service ensures long-term value over short-term cost savings by investing in proven accuracy, regulatory expertise, and automation capabilities that reduce administrative burden and mitigate risk. This strategic approach helps align vendor capabilities with organizational goals, whether for health plans managing provider networks, healthcare systems credentialing medical staff, or specialty providers ensuring regulatory compliance.
Verisys stands as the trusted partner for healthcare credentialing, offering real-time verified data, continuous monitoring, and seamless integration to help healthcare organizations optimize credentialing procedures and maintain industry standards. By choosing the right vendor, you can focus on what matters most: delivering quality patient care while protecting your organization from legal and financial exposure.
Sources
- NCQA. FAQ Directory: Health Plan Accreditation. https://www.ncqa.org/programs/health-plans/health-plan-accreditation-hpa/faqs/all/?faq=000025418
- CAQH. The CAQH Index Report. https://www.caqh.org/insights/caqh-index-report
- U.S. Department of Health & Human Services, HRSA, NPDB. NPDB Insights – March 2024. https://www.npdb.hrsa.gov/enews/March2024Insights.jsp
- MGMA. Confronting Credentialing, Reappointment Crunch Time in Your Medical Practice. https://www.mgma.com/mgma-stat/confronting-credentialing-reappointment-crunch-time