Provider Credentialing Management Solutions
For three decades, healthcare, life science, and medical background screening organizations have depended on Verisys for access to the complete range of provider credentialing and workforce data management services.
Empowering Healthcare Organizations With Data and Technology Solutions
FACIS®
FACIS delivers 360-degree transparency on providers, staff, and entities for the medical organizations who hire, credential, refer, and reimburse for healthcare delivery.
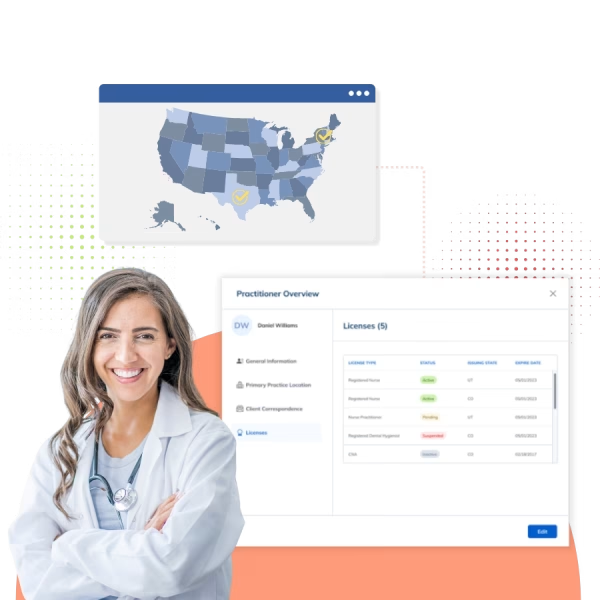
License Verification
Point-in-time license verification with real-time alerts regarding status, issue date, expiration date, primary source information, and any disciplinary action (current or historical) using network information.

Credentialing
Verisys is the largest outsourced CVO on the market today and the only player with the workflow service expertise and in-house database (i.e., FACIS) to serve the end-to-end needs of large healthcare organizations efficiently. Our advanced systems ensure that every aspect of the provider credentialing process is covered.

Workforce Management
Verisys’ Provider Directory Management Solutions transform often-flawed information into comprehensive, customizable directories that integrate seamlessly with your member portal. Verisys helps organizations maintain up-to-date and reliable directories.

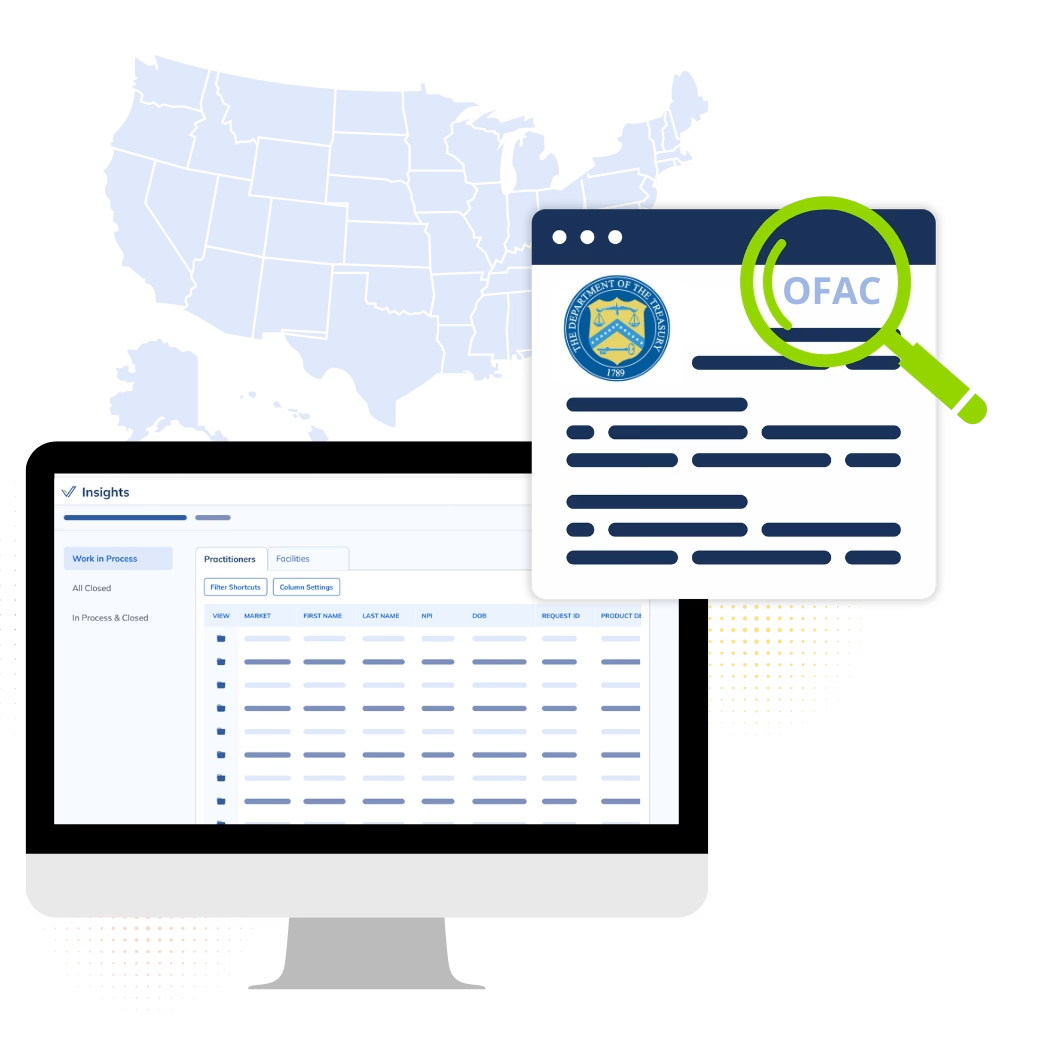
Ongoing Monitoring
Continuous healthcare compliance monitoring for medical practitioners adds a layer of security and ensures ongoing compliance with care regulations. This ongoing process minimizes regulatory risks, streamlines audits, and reinforces adherence to evolving healthcare standards.
Pre to Post Hire Screening
Industry leader in medical background checks and pre-hire screening, Verisys helps healthcare organizations maintain compliance with current health standards and safeguard against fraud and abuse. By leveraging comprehensive credentialing and provider verification, we ensure that only qualified healthcare practitioners are hired, minimizing risks and protecting patients.
Addressing Common Credentialing Hurdles
Healthcare providers and organizations frequently face challenges such as delays caused by inaccurate or incomplete physician, nurse, or other medical practitioner information during the credentialing process. Automated network services can effectively address these obstacles by minimizing document paperwork and optimizing process workflows. This provider credentialing automation not only accelerates medical data verification but also reduces healthcare application processing times. Additionally, consistent training for staff on current state and federal qualification requirements ensures the credentialing process maintains its integrity, helping prevent compliance issues and safeguarding the overall quality of care.














