– The best resource for monthly healthcare regulatory compliance updates. Compliance Updates: April 2024 Overlook: Licensure Compacts Other Legislation Board Updates Interstate Medical...

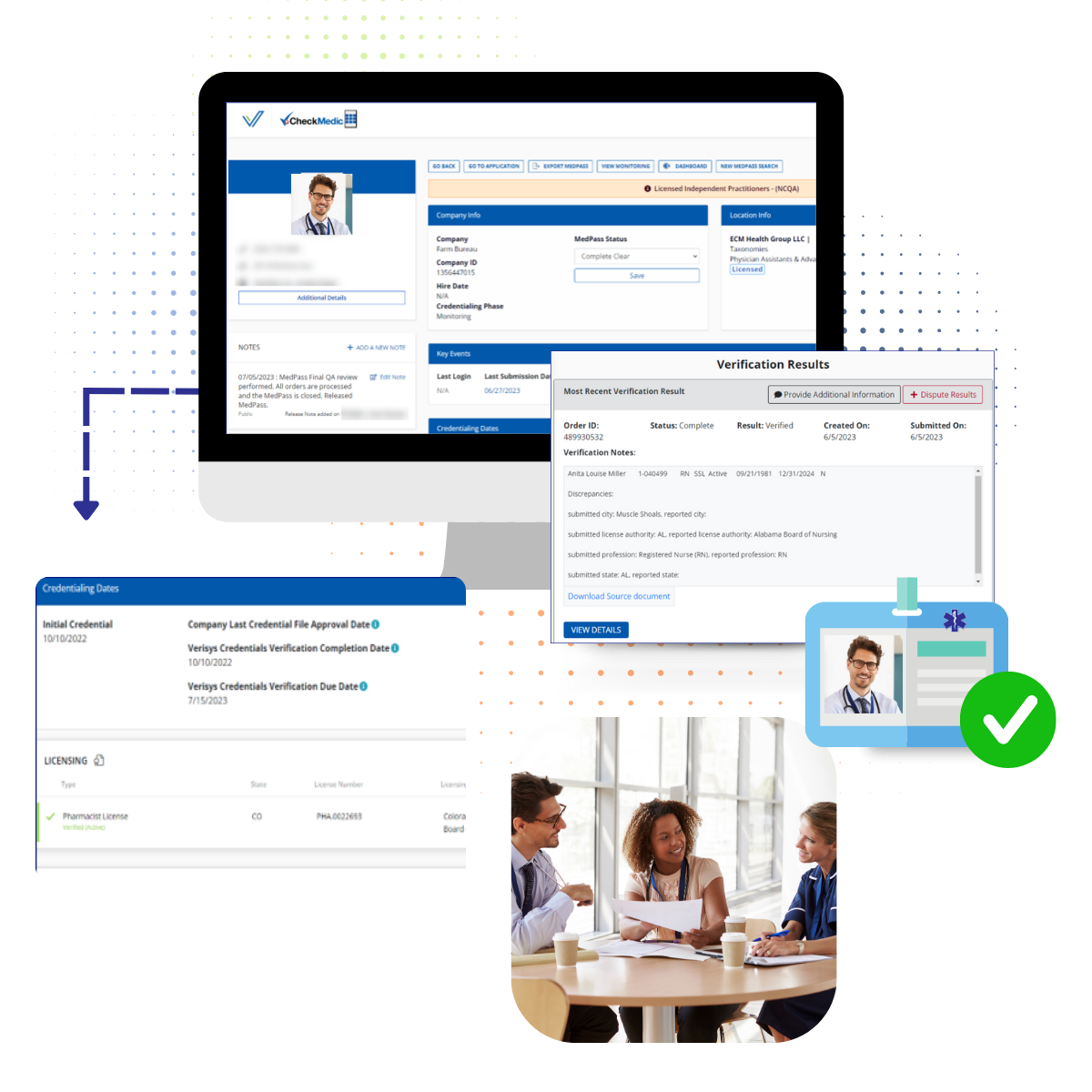
Leverage data-rich tools and longitudinal provider profiles to streamline processes, accelerate verifications, and enable compliant, aligned provider networks .
Health plans need a secure, efficient, and trusted source for provider data that mitigates risk, lowers operational costs, and streamlines network administration functions so you can focus on delivering quality care and achieving optimal outcomes. Failure in either area creates the potential for significant fines for non-compliance, litigation risk, payment/billing issues and reputational damage.
Verisys is an industry leader in provider credentialing, leveraging data-rich tools and longitudinal provider profiles, streamlining:
For hundreds of healthcare payers and related stakeholders across all sides of the industry.
Clients include:
Streamline network administration with our configurable payer credentialing solutions and up-to-the-minute provider directories powered by accurate, verified data.
Verisys is the largest outsourced credentialing provider in the market today and the only player with the workflow expertise and in-house database (i.e., FACIS) to efficiently serve the end-to-end needs of large healthcare clients. For three decades, Verisys has supported client components of network management to ensure regulatory compliance and enable payors to keep an up-to-date provider network. Verisys credentialing is the only NCQA and URAC accredited solution to maintain the industry’s highest data and compliance standards.
Verisys can do simple provider credential searches OR implement a full end-to-end credentialing solution.

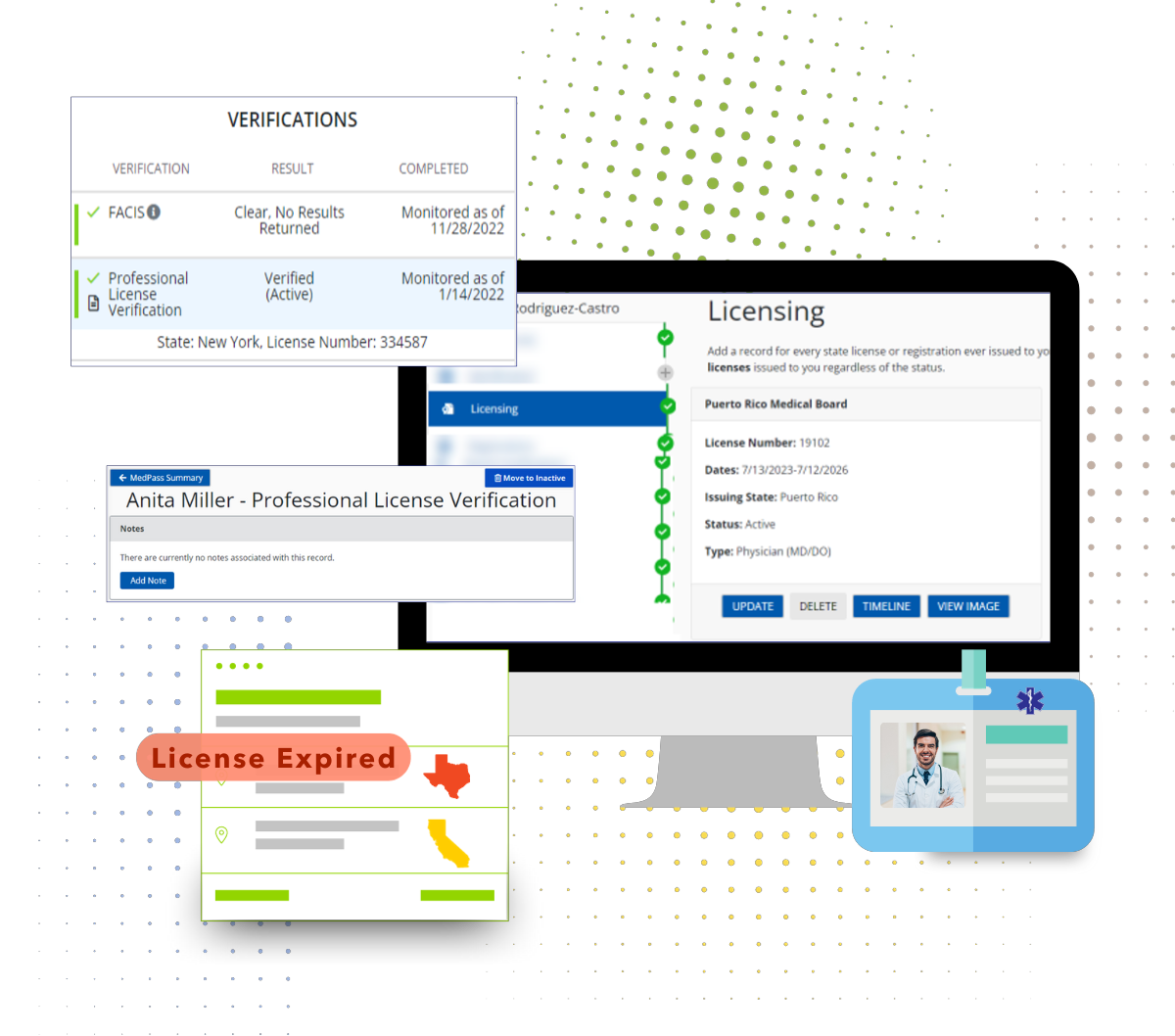
Provide a point-in-time license verification of a professional license number, including status, issue and expiration date, primary source information, and any disciplinary action (current or historical). Searches aliases provided on each practitioner as part of the search criteria and verification process
Faster license verification to accelerate efficiency and reduce fraud and waste.
Verisys’ Provider Directory Management Solutions transform often flawed provider data into comprehensive, customizable directories that integrate seamlessly with your member portal. We display intricate networks how you want your members to see them, highlighting and tiering network providers just for them — including telemedicine providers.
By delivering relevant, actionable information, consumers can make informed decisions leading to better outcomes—one of healthcare reform’s primary goals.
By offering a more comprehensive, integrated provider search platform, you can keep current members satisfied and engaged while attracting new customers who want to strengthen member engagement.

Continuously monitoring your population adds a layer of security and makes ongoing compliance with regulations set by standard-setting bodies possible. To stay in compliance with federal and state regulations and to keep patients safe, it’s vital for hospitals and health systems to monitor the licenses of their practitioners for new information that may prevent a physician from practicing. If a practitioner’s license is invalid, suspended, or expired, or if restrictions are placed on a license, healthcare organizations must take steps to halt the treatment of patients until the practitioner gets his license back in good standing.
The best way to ensure all practitioner licenses remain in good standing is through continuous healthcare license monitoring.
FACIS® is the industry’s most comprehensive database consisting of primary content from federal and state sources for exclusions, sanctions, debarments, disciplinary actions, and adverse events against healthcare professionals and entities for all 868 taxonomies and all 56 U.S. states and jurisdictions. A database of over 10 million records from over 3,500 primary sources on provider exclusions, sanctions, and adverse events, FACIS® delivers 360-degree transparency on providers, staff, and entities for the organizations who hire, credential, refer, and reimburse for healthcare delivery.
When it comes to keeping customers and patients safe, you need the gold standard.

READY TO STREAMLINE Your Compliance?
Let Verisys optimize payer network functions including credentialing, employee monitoring and provider network data augmentation through technology and data.