– The best resource for monthly healthcare regulatory compliance updates. Compliance Updates: April 2024 Overlook: Licensure Compacts Other Legislation Board Updates Interstate Medical...

The Health Plan Accreditation National Summit was held on February 19 – 20 in Las Vegas, NV. Health Plan Accreditation (HPA) professionals, healthcare payer organizations, consultants serving health plans, and software solution providers from around the country gathered for this two-day event. These professionals shared with one another the tools and processes they have in place to optimize their results, successes the plans are having and how they are achieving them, and information about NCQA’s new 2020 updates.
Key topics covered at the conference included the following:
Why Health Plan Accreditation?
According to NCQA, there are several important reasons for health plans to gain accreditation:
NCQA Health Plan Accreditation Helps Health Plans Meet Their Goals
The National Committee for Quality Assurance (NCQA) was established to measure quality and to improve health care. NCQA Health Plan Accreditation provides the framework for health plans to support care that keeps members at optimum levels of health while also controlling costs and meeting government and purchaser requirements.
NCQA Health Plan Accreditation builds upon more than 25 years of experience to provide a rigorous and comprehensive framework for quality improvement and measurement. It is the only program in the industry that bases results on clinical performance and consumer experience (HEDIS® and CAHPS®). NCQA standards are a roadmap for improvement—organizations use them to perform a gap analysis and align improvement activities with areas that are most important to states and employers.
NCQA Standards Evaluate Plans On:
NCQA’s New 2020 Star Rating System for Accreditation
Every year NCQA makes adjustments to its standards to respond to feedback from health plans, policymakers, providers, patients, and others. In 2020, in addition to modifications to the standards, NCQA made updates to how they score and award accreditation to create a more straight forward and transparent process while maintaining strong consumer protections.
The NCQA Adjustments Made in 2020 Focus on the Following Areas:
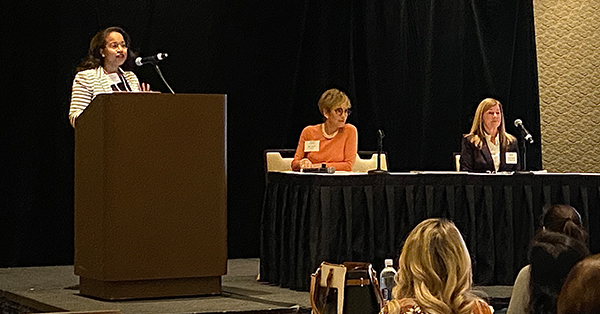
Verisys Presents with AmeriHealth Caritas
Verisys presented with Susan Adams, Director of Corporate Credentialing, and Keysa Shaw Sanders, Manager of Enterprise Accreditation Programs, both from AmeriHealth Caritas, on Success with Credentialing and Network Management Standards.
Susan focused on the NCQA standards and explained the “must-pass” elements added in 2020. Keysa talked about network controls and provider network management standards. Verisys explained the importance of looking at the providers coming into your network, addressing the issues of qualifying the providers, and how that affects patient safety, patient outcomes, costs, your plan’s reputation, and the controls you have in place. This session, as well as the other presentations throughout the conference, offered proven strategies for success that plans can take back and put to use. Many of the sessions were designed to give the health plans a roadmap for success to use for future reviews, surveys, and audits.
Verisys is a Credentials Verification Organization dedicated to improving the quality of health care in the U.S. by ensuring health care providers within your network are thoroughly screened and credentialed which reduces fraud, waste, and abuse in the health care system. Properly credentialing your network providers also assists in the accreditation process keeping you in full compliance.
 |
Written by Juliette Willard Healthcare Communications Specialist Being creative is my passion! Writer. Painter. Problem Solver. Optimist. Connect with Juliette on LinkedIn |