– The best resource for monthly healthcare regulatory compliance updates. Compliance Updates: April 2024 Overlook: Licensure Compacts Other Legislation Board Updates Interstate Medical...

15,000,000+
Background Screening Searches Annually
8,000,000+
Providers Monitored Annually
2,200,000+
Credentialing Events Annually
Empowering Healthcare Organizations With Data and Technology Solutions
FACIS® delivers 360-degree transparency on providers, staff, and entities for the organizations who hire, credential, refer, and reimburse for healthcare delivery.

Point-in-time license verification of professional license numbers, including status, issue/expiration date, primary source information, and any disciplinary action (current or historical).

We are the largest outsourced credentialing provider in the market today & only player with the expertise and in-house data to efficiently serve end-to-end needs of large healthcare clients.

Verisys’ Provider Management Solutions transform provider data into comprehensive, customizable directories that integrate seamlessly with your member portal.

Continuously monitor your population for added security & compliance with federal and state regulations to keep patients safe.

Industry leader in pre-hire screening. Maintain compliance and safeguard against fraud and abuse.

Verify up-to-date, compliant status on NPI, DEA, Medice Opt Out, Federal Exclusions, State Exclusions, PECOS, and State Licensing Boards.
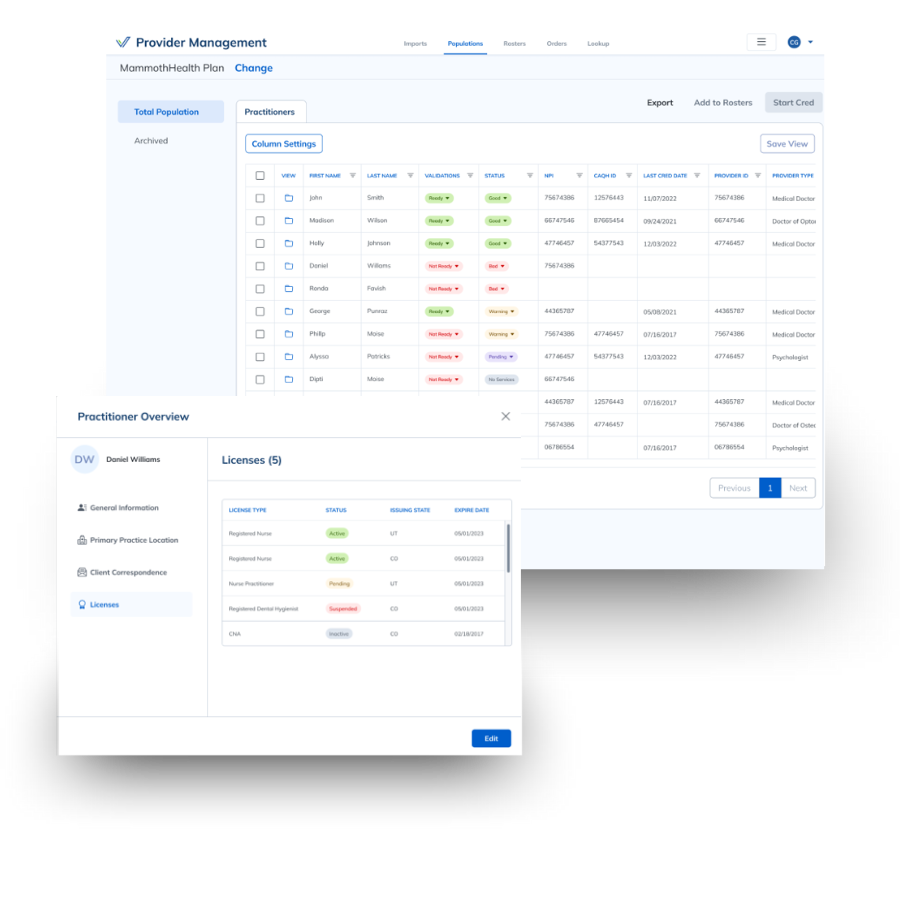
Verisys can support in-house credentialing with automated realtime verifications, which can be integrated into internal processing systems.

Monitor licensure, DEA, SSA-DMF, FACIS (sanctions, exclusions, debarments, license disciplinary action), controlled substance registration, and certifications.
Identify Fraud & Reduce Organizational Risk
We Hear the Problems…
I do not want bad actors to put my business at risk
Fines from CMS begin at $10K and quickly escalate based on the provider or pharmacist interactions with patients
I need to expand quickly into new markets
I need to make sure our constituents have access to the right providers!
But I also need to make the enrollment process easy. Doctors are busy and should be helping patients!
500,000,000+
Sanction & Adverse Event Records
32+
Years Serving Healthcare Orgs Nationwide
Hundreds of Health Plans, Retail Pharmacies, Life Science Companies, Background Screeners, Hospitals and Health Systems, and State and Federal Government Entities, have found success with Verisys solutions.
(Feedback From 2022 NPS Survey)